
Pulmonology (Lungs)
Recent Blogs
Pulmonary Conditions We Treat in New Prague
Our pulmonology team has the knowledge and skills to diagnose and treat the following pulmonary conditions and diseases:
-
Asthma
If you have asthma, the inside walls of the airways in your lungs can become inflamed and swollen. In addition, membranes in your airway linings may secrete excess mucus. The result is an asthma attack. During an asthma attack, your narrowed airways make it harder to breathe, and you may cough and wheeze.

-
Bronchopulmonary Dysplasia (BPD)
A form of chronic lung disease that affects premature babies and infants from damage to the lungs caused by mechanical ventilation (respirator) and long-term use of oxygen. Most infants recover, but some may have long-term breathing problems. -
Chronic Bronchitis
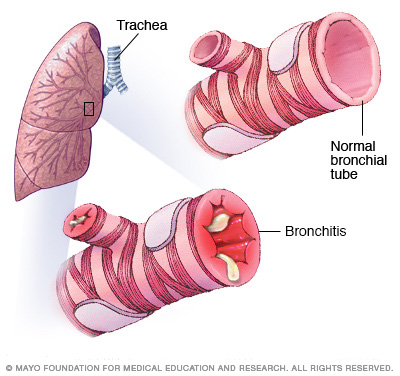 Bronchitis is an inflammation of the lining of your bronchial tubes, which carry air to and from your lungs. People who have bronchitis often cough up thickened mucus, which can be discolored. Bronchitis may be either acute or chronic.
Bronchitis is an inflammation of the lining of your bronchial tubes, which carry air to and from your lungs. People who have bronchitis often cough up thickened mucus, which can be discolored. Bronchitis may be either acute or chronic.
Often developing from a cold or other respiratory infection, acute bronchitis is very common. Chronic bronchitis, a more serious condition, is a constant irritation or inflammation of the lining of the bronchial tubes, often due to smoking.
Acute bronchitis, also called a chest cold, usually improves within a week to 10 days without lasting effects, although the cough may linger for weeks.
However, if you have repeated bouts of bronchitis, you may have chronic bronchitis, which requires medical attention. Chronic bronchitis is one of the conditions included in chronic obstructive pulmonary disease (COPD).
Symptoms
For either acute bronchitis or chronic bronchitis, signs and symptoms may include:
- Cough
- Production of mucus (sputum), which can be clear, white, yellowish-gray or green in color — rarely, it may be streaked with blood
- Fatigue
- Shortness of breath
- Slight fever and chills
- Chest discomfort
If you have acute bronchitis, you might have cold symptoms, such as a mild headache or body aches. While these symptoms usually improve in about a week, you may have a nagging cough that lingers for several weeks.
Chronic bronchitis is defined as a productive cough that lasts at least three months, with recurring bouts occurring for at least two consecutive years.
If you have chronic bronchitis, you're likely to have periods when your cough or other symptoms worsen. At those times, you may have an acute infection on top of chronic bronchitis.
When to see a doctor
See your doctor if your cough:
- Lasts more than three weeks
- Prevents you from sleeping
- Is accompanied by fever higher than 100.4 F (38 C)
- Produces discolored mucus
- Produces blood
- Is associated with wheezing or shortness of breath
Causes
Acute bronchitis is usually caused by viruses, typically the same viruses that cause colds and flu (influenza). Antibiotics don't kill viruses, so this type of medication isn't useful in most cases of bronchitis.
The most common cause of chronic bronchitis is cigarette smoking. Air pollution and dust or toxic gases in the environment or workplace also can contribute to the condition.
Risk factors
Factors that increase your risk of bronchitis include:
- Cigarette smoke. People who smoke or who live with a smoker are at higher risk of both acute bronchitis and chronic bronchitis.
- Low resistance. This may result from another acute illness, such as a cold, or from a chronic condition that compromises your immune system. Older adults, infants and young children have greater vulnerability to infection.
- Exposure to irritants on the job. Your risk of developing bronchitis is greater if you work around certain lung irritants, such as grains or textiles, or are exposed to chemical fumes.
- Gastric reflux. Repeated bouts of severe heartburn can irritate your throat and make you more prone to developing bronchitis.
Complications
Although a single episode of bronchitis usually isn't cause for concern, it can lead to pneumonia in some people. Repeated bouts of bronchitis, however, may mean that you have chronic obstructive pulmonary disease (COPD).
Prevention
To reduce your risk of bronchitis, follow these tips:
- Avoid cigarette smoke. Cigarette smoke increases your risk of chronic bronchitis.
- Get vaccinated. Many cases of acute bronchitis result from influenza, a virus. Getting a yearly flu vaccine can help protect you from getting the flu. You may also want to consider vaccination that protects against some types of pneumonia.
- Wash your hands. To reduce your risk of catching a viral infection, wash your hands frequently and get in the habit of using alcohol-based hand sanitizers.
- Wear a surgical mask. If you have COPD, you might consider wearing a face mask at work if you're exposed to dust or fumes, and when you're going to be among crowds, such as while traveling.
-
Chronic Obstructive Pulmonary Disease (COPD)
Chronic obstructive pulmonary disease (COPD) is a chronic inflammatory lung disease that causes obstructed airflow from the lungs. Symptoms include breathing difficulty, cough, mucus (sputum) production and wheezing. It's caused by long-term exposure to irritating gases or particulate matter, most often from cigarette smoke. People with COPD are at increased risk of developing heart disease, lung cancer and a variety of other conditions.
Emphysema and chronic bronchitis are the two most common conditions that contribute to COPD. Chronic bronchitis is inflammation of the lining of the bronchial tubes, which carry air to and from the air sacs (alveoli) of the lungs. It's characterized by daily cough and mucus (sputum) production.
Emphysema is a condition in which the alveoli at the end of the smallest air passages (bronchioles) of the lungs are destroyed as a result of damaging exposure to cigarette smoke and other irritating gases and particulate matter.
COPD is treatable. With proper management, most people with COPD can achieve good symptom control and quality of life, as well as reduced risk of other associated conditions.
Symptoms
COPD symptoms often don't appear until significant lung damage has occurred, and they usually worsen over time, particularly if smoking exposure continues. For chronic bronchitis, the main symptom is a daily cough and mucus (sputum) production at least three months a year for two consecutive years.
Other signs and symptoms of COPD may include:
- Shortness of breath, especially during physical activities
- Wheezing
- Chest tightness
- Having to clear your throat first thing in the morning, due to excess mucus in your lungs
- A chronic cough that may produce mucus (sputum) that may be clear, white, yellow or greenish
- Blueness of the lips or fingernail beds (cyanosis)
- Frequent respiratory infections
- Lack of energy
- Unintended weight loss (in later stages)
- Swelling in ankles, feet or legs
People with COPD are also likely to experience episodes called exacerbations, during which their symptoms become worse than usual day-to-day variation and persist for at least several days.
Causes
The main cause of COPD in developed countries is tobacco smoking. In the developing world, COPD often occurs in people exposed to fumes from burning fuel for cooking and heating in poorly ventilated homes.
Only about 20 to 30 percent of chronic smokers may develop clinically apparent COPD, although many smokers with long smoking histories may develop reduced lung function. Some smokers develop less common lung conditions. They may be misdiagnosed as having COPD until a more thorough evaluation is performed.
How your lungs are affected
Air travels down your windpipe (trachea) and into your lungs through two large tubes (bronchi). Inside your lungs, these tubes divide many times — like the branches of a tree — into many smaller tubes (bronchioles) that end in clusters of tiny air sacs (alveoli).
The air sacs have very thin walls full of tiny blood vessels (capillaries). The oxygen in the air you inhale passes into these blood vessels and enters your bloodstream. At the same time, carbon dioxide — a gas that is a waste product of metabolism — is exhaled.
Your lungs rely on the natural elasticity of the bronchial tubes and air sacs to force air out of your body. COPD causes them to lose their elasticity and overexpand, which leaves some air trapped in your lungs when you exhale.
Causes of airway obstruction
Causes of airway obstruction include:
- Emphysema. This lung disease causes destruction of the fragile walls and elastic fibers of the alveoli. Small airways collapse when you exhale, impairing airflow out of your lungs.
- Chronic bronchitis. In this condition, your bronchial tubes become inflamed and narrowed and your lungs produce more mucus, which can further block the narrowed tubes. You develop a chronic cough trying to clear your airways.
Cigarette smoke and other irritants
In the vast majority of cases, the lung damage that leads to COPD is caused by long-term cigarette smoking. But there are likely other factors at play in the development of COPD, such as a genetic susceptibility to the disease, because only about 20 to 30 percent of smokers may develop COPD.
Other irritants can cause COPD, including cigar smoke, secondhand smoke, pipe smoke, air pollution and workplace exposure to dust, smoke or fumes.
Alpha-1-antitrypsin deficiency
In about 1 percent of people with COPD, the disease results from a genetic disorder that causes low levels of a protein called alpha-1-antitrypsin. Alpha-1-antitrypsin (AAt) is made in the liver and secreted into the bloodstream to help protect the lungs. Alpha-1-antitrypsin deficiency can affect the liver as well as the lungs. Damage to the lung can occur in infants and children, not only adults with long smoking histories.
For adults with COPD related to AAt deficiency, treatment options include those used for people with more-common types of COPD. In addition, some people can be treated by replacing the missing AAt protein, which may prevent further damage to the lungs.
Risk factors
Risk factors for COPD include:
- Exposure to tobacco smoke. The most significant risk factor for COPD is long-term cigarette smoking. The more years you smoke and the more packs you smoke, the greater your risk. Pipe smokers, cigar smokers and marijuana smokers also may be at risk, as well as people exposed to large amounts of secondhand smoke.
- People with asthma who smoke. The combination of asthma, a chronic inflammatory airway disease, and smoking increases the risk of COPD even more.
- Occupational exposure to dusts and chemicals. Long-term exposure to chemical fumes, vapors and dusts in the workplace can irritate and inflame your lungs.
- Exposure to fumes from burning fuel. In the developing world, people exposed to fumes from burning fuel for cooking and heating in poorly ventilated homes are at higher risk of developing COPD.
- Age. COPD develops slowly over years, so most people are at least 40 years old when symptoms begin.
- Genetics. The uncommon genetic disorder alpha-1-antitrypsin deficiency is the cause of some cases of COPD. Other genetic factors likely make certain smokers more susceptible to the disease.
Complications
COPD can cause many complications, including:
- Respiratory infections. People with COPD are more likely to catch colds, the flu and pneumonia. Any respiratory infection can make it much more difficult to breathe and could cause further damage to lung tissue. An annual flu vaccination and regular vaccination against pneumococcal pneumonia can prevent some infections.
- Heart problems. For reasons that aren't fully understood, COPD can increase your risk of heart disease, including heart attack. Quitting smoking may reduce this risk.
- Lung cancer. People with COPD have a higher risk of developing lung cancer. Quitting smoking may reduce this risk.
- High blood pressure in lung arteries. COPD may cause high blood pressure in the arteries that bring blood to your lungs (pulmonary hypertension).
- Depression. Difficulty breathing can keep you from doing activities that you enjoy. And dealing with serious illness can contribute to development of depression. Talk to your doctor if you feel sad or helpless or think that you may be experiencing depression.
Prevention
Unlike some diseases, COPD has a clear cause and a clear path of prevention. The majority of cases are directly related to cigarette smoking, and the best way to prevent COPD is to never smoke — or to stop smoking now.
If you're a longtime smoker, these simple statements may not seem so simple, especially if you've tried quitting — once, twice or many times before. But keep trying to quit. It's critical to find a tobacco cessation program that can help you quit for good. It's your best chance for preventing damage to your lungs.
Occupational exposure to chemical fumes and dust is another risk factor for COPD. If you work with this type of lung irritant, talk to your supervisor about the best ways to protect yourself, such as using respiratory protective equipment.
-
Cystic Fibrosis
Cystic fibrosis is an inherited disorder that causes severe damage to the lungs, digestive system and other organs in the body.
Cystic fibrosis affects the cells that produce mucus, sweat and digestive juices. These secreted fluids are normally thin and slippery. But in people with cystic fibrosis, a defective gene causes the secretions to become sticky and thick. Instead of acting as a lubricant, the secretions plug up tubes, ducts and passageways, especially in the lungs and pancreas.
Although cystic fibrosis requires daily care, people with the condition are usually able to attend school and work, and often have a better quality of life than people with cystic fibrosis had in previous decades. Improvements in screening and treatments mean people with cystic fibrosis now may live into their mid- to late 30s, on average, and some are living into their 40s and 50s.
Symptoms
Screening of newborns for cystic fibrosis is now performed in every state in the United States. As a result, the condition can be diagnosed within the first month of life, before symptoms develop. For people born before newborn screening was performed, it's important to be aware of the signs and symptoms of cystic fibrosis.
Cystic fibrosis signs and symptoms vary, depending on the severity of the disease. Even in the same person, symptoms may worsen or improve as time passes. Some people may not experience symptoms until adolescence or adulthood.
People with cystic fibrosis have a higher than normal level of salt in their sweat. Parents often can taste the salt when they kiss their children. Most of the other signs and symptoms of cystic fibrosis affect the respiratory system and digestive system. However, adults diagnosed with cystic fibrosis are more likely to have atypical symptoms, such as recurring bouts of inflamed pancreas (pancreatitis), infertility and recurring pneumonia.
Respiratory signs and symptoms
The thick and sticky mucus associated with cystic fibrosis clogs the tubes that carry air in and out of your lungs. This can cause signs and symptoms such as:
- A persistent cough that produces thick mucus (sputum)
- Wheezing
- Breathlessness
- Exercise intolerance
- Repeated lung infections
- Inflamed nasal passages or a stuffy nose
Digestive signs and symptoms
The thick mucus can also block tubes that carry digestive enzymes from your pancreas to your small intestine. Without these digestive enzymes, your intestines aren't able to completely absorb the nutrients in the food you eat. The result is often:
- Foul-smelling, greasy stools
- Poor weight gain and growth
- Intestinal blockage, particularly in newborns (meconium ileus)
- Severe constipation
Frequent straining while passing stool can cause part of the rectum — the end of the large intestine — to protrude outside the anus (rectal prolapse). When this occurs in children, it may be a sign of cystic fibrosis. Parents should consult a physician knowledgeable about cystic fibrosis. Rectal prolapse in children may sometimes require surgery. Rectal prolapse in children with cystic fibrosis is less common than it was in the past, which may be due to earlier testing, diagnosis and treatment of cystic fibrosis.
When to see a doctor
If you or your child has symptoms of cystic fibrosis — or if someone in your family has cystic fibrosis — talk with your doctor about testing for the disease.
Seek immediate medical care if you or your child has difficulty breathing.
Causes
In cystic fibrosis, a defect (mutation) in a gene changes a protein that regulates the movement of salt in and out of cells. The result is thick, sticky mucus in the respiratory, digestive and reproductive systems, as well as increased salt in sweat.
Many different defects can occur in the gene. The type of gene mutation is associated with the severity of the condition.
Children need to inherit one copy of the gene from each parent in order to have the disease. If children inherit only one copy, they won't develop cystic fibrosis. However, they will be carriers and possibly pass the gene to their own children.
Risk factors
- Family history. Because cystic fibrosis is an inherited disorder, it runs in families.
- Race. Although cystic fibrosis occurs in all races, it is most common in white people of Northern European ancestry.
Complications
Respiratory system complications
- Damaged airways (bronchiectasis). Cystic fibrosis is one of the leading causes of bronchiectasis, a condition that damages the airways. This makes it harder to move air in and out of the lungs and clear mucus from the airways (bronchial tubes).
- Chronic infections. Thick mucus in the lungs and sinuses provides an ideal breeding ground for bacteria and fungi. People with cystic fibrosis may often have sinus infections, bronchitis or pneumonia.
- Growths in the nose (nasal polyps). Because the lining inside the nose is inflamed and swollen, it can develop soft, fleshy growths (polyps).
- Coughing up blood (hemoptysis). Over time, cystic fibrosis can cause thinning of the airway walls. As a result, teenagers and adults with cystic fibrosis may cough up blood.
- Pneumothorax. This condition, in which air collects in the space that separates the lungs from the chest wall, also is more common in older people with cystic fibrosis. Pneumothorax can cause chest pain and breathlessness.
- Respiratory failure. Over time, cystic fibrosis can damage lung tissue so badly that it no longer works. Lung function usually worsens gradually, and it eventually can become life-threatening.
- Acute exacerbations. People with cystic fibrosis may experience worsening of their respiratory symptoms, such as coughing and shortness of breath, for several days to weeks. This is called an acute exacerbation and requires treatment in the hospital.
Digestive system complications
- Nutritional deficiencies. Thick mucus can block the tubes that carry digestive enzymes from your pancreas to your intestines. Without these enzymes, your body can't absorb protein, fats or fat-soluble vitamins.
- Diabetes. The pancreas produces insulin, which your body needs to use sugar. Cystic fibrosis increases the risk of diabetes. Around 30 percent of people with cystic fibrosis develop diabetes by age 30.
- Blocked bile duct. The tube that carries bile from your liver and gallbladder to your small intestine may become blocked and inflamed, leading to liver problems and sometimes gallstones. Intestinal obstruction.
- Intestinal obstruction can happen to people with cystic fibrosis at all ages. Children and adults with cystic fibrosis are more likely than are infants to develop intussusception, a condition in which a section of the intestines folds in on itself like an accordion.
- Distal intestinal obstruction syndrome (DIOS). DIOS is partial or complete obstruction where the small intestine meets the large intestine.
Reproductive system complications
Almost all men with cystic fibrosis are infertile because the tube that connects the testes and prostate gland (vas deferens) is either blocked with mucus or missing entirely. Certain fertility treatments and surgical procedures sometimes make it possible for men with cystic fibrosis to become biological fathers.
Although women with cystic fibrosis may be less fertile than other women, it's possible for them to conceive and to have successful pregnancies. Still, pregnancy can worsen the signs and symptoms of cystic fibrosis, so be sure to discuss the possible risks with your doctor.
Other complications
- Thinning of the bones (osteoporosis). People with cystic fibrosis are at higher risk of developing a dangerous thinning of bones.
- Electrolyte imbalances and dehydration. Because people with cystic fibrosis have saltier sweat, the balance of minerals in their blood may be upset. Signs and symptoms include increased heart rate, fatigue, weakness and low blood pressure.
Prevention
If you or your partner has close relatives with cystic fibrosis, you both may want to undergo genetic testing before having children. The test, which is performed in a lab on a sample of blood, can help determine your risk of having a child with cystic fibrosis.
If you're already pregnant and the genetic test shows that your baby may be at risk of cystic fibrosis, your doctor can conduct additional tests on your developing child.
Genetic testing isn't for everyone. Before you decide to be tested, you should talk to a genetic counselor about the psychological impact the test results might carry.
-
Emphysema
Emphysema is a lung condition that causes shortness of breath. In people with emphysema, the air sacs in the lungs (alveoli) are damaged. Over time, the inner walls of the air sacs weaken and rupture — creating larger air spaces instead of many small ones. This reduces the surface area of the lungs and, in turn, the amount of oxygen that reaches your bloodstream.
When you exhale, the damaged alveoli don't work properly and old air becomes trapped, leaving no room for fresh, oxygen-rich air to enter.
Most people with emphysema also have chronic bronchitis. Chronic bronchitis is inflammation of the tubes that carry air to your lungs (bronchial tubes), which leads to a persistent cough.
Emphysema and chronic bronchitis are two conditions that make up chronic obstructive pulmonary disease (COPD). Smoking is the leading cause of COPD. Treatment may slow the progression of COPD, but it can't reverse the damage.
Symptoms
You can have emphysema for many years without noticing any signs or symptoms. The main symptom of emphysema is shortness of breath, which usually begins gradually.
You may start avoiding activities that cause you to be short of breath, so the symptom doesn't become a problem until it starts interfering with daily tasks. Emphysema eventually causes shortness of breath even while you're at rest.
When to see a doctor
See your doctor if you've had unexplained shortness of breath for several months, especially if it's getting worse or it's interfering with your daily activities. Don't ignore it by telling yourself it's because you're aging or out of shape. Seek immediate medical attention if:
- You're so short of breath, you can't climb stairs
- Your lips or fingernails turn blue or gray with exertion
- You're not mentally alert
Causes
The main cause of emphysema is long-term exposure to airborne irritants, including:
- Tobacco smoke
- Marijuana smoke
- Air pollution
- Chemical fumes and dust
Rarely, emphysema is caused by an inherited deficiency of a protein that protects the elastic structures in the lungs. It's called alpha-1-antitrypsin deficiency emphysema.
Risk factors
Factors that increase your risk of developing emphysema include:
- Smoking. Emphysema is most likely to develop in cigarette smokers, but cigar and pipe smokers also are susceptible. The risk for all types of smokers increases with the number of years and amount of tobacco smoked.
- Age. Although the lung damage that occurs in emphysema develops gradually, most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60.
- Exposure to secondhand smoke. Secondhand smoke, also known as passive or environmental tobacco smoke, is smoke that you inadvertently inhale from someone else's cigarette, pipe or cigar. Being around secondhand smoke increases your risk of emphysema.
- Occupational exposure to fumes or dust. If you breathe fumes from certain chemicals or dust from grain, cotton, wood or mining products, you're more likely to develop emphysema. This risk is even greater if you smoke.
- Exposure to indoor and outdoor pollution. Breathing indoor pollutants, such as fumes from heating fuel, as well as outdoor pollutants — car exhaust, for instance — increases your risk of emphysema.
Complications
People who have emphysema are also more likely to develop:
- Collapsed lung (pneumothorax). A collapsed lung can be life-threatening in people who have severe emphysema, because the function of their lungs is already so compromised. This is uncommon but serious when it occurs.
- Heart problems. Emphysema can increase the pressure in the arteries that connect the heart and lungs. This can cause a condition called cor pulmonale, in which a section of the heart expands and weakens.
- Large holes in the lungs (bullae). Some people with emphysema develop empty spaces in the lungs called bullae. They can be as large as half the lung. In addition to reducing the amount of space available for the lung to expand, giant bullae can increase your risk of pneumothorax.
Prevention
To prevent emphysema, don't smoke and avoid breathing secondhand smoke. Wear a mask to protect your lungs if you work with chemical fumes or dust.
-
High Blood Pressure (Hypertension)
High blood pressure is a common condition in which the long-term force of the blood against your artery walls is high enough that it may eventually cause health problems, such as heart disease.
Blood pressure is determined both by the amount of blood your heart pumps and the amount of resistance to blood flow in your arteries. The more blood your heart pumps and the narrower your arteries, the higher your blood pressure.
You can have high blood pressure (hypertension) for years without any symptoms. Even without symptoms, damage to blood vessels and your heart continues and can be detected. Uncontrolled high blood pressure increases your risk of serious health problems, including heart attack and stroke.
High blood pressure generally develops over many years, and it affects nearly everyone eventually. Fortunately, high blood pressure can be easily detected. And once you know you have high blood pressure, you can work with your doctor to control it.
Symptoms
Most people with high blood pressure have no signs or symptoms, even if blood pressure readings reach dangerously high levels.
A few people with high blood pressure may have headaches, shortness of breath or nosebleeds, but these signs and symptoms aren't specific and usually don't occur until high blood pressure has reached a severe or life-threatening stage.
When to see a doctor
You'll likely have your blood pressure taken as part of a routine doctor's appointment.
Ask your doctor for a blood pressure reading at least every two years starting at age 18. If you're age 40 or older, or you're age 18-39 with a high risk of high blood pressure, ask your doctor for a blood pressure reading every year. Blood pressure generally should be checked in both arms to determine if there is a difference. It's important to use an appropriate-sized arm cuff. Your doctor will likely recommend more frequent readings if you've already been diagnosed with high blood pressure or have other risk factors for cardiovascular disease. Children age 3 and older will usually have blood pressure measured as a part of their yearly checkups.
If you don't regularly see your doctor, you may be able to get a free blood pressure screening at a health resource fair or other locations in your community. You can also find machines in some stores that will measure your blood pressure for free.
Public blood pressure machines, such as those found in pharmacies, may provide helpful information about your blood pressure, but they may have some limitations. The accuracy of these machines depends on several factors, such as a correct cuff size and proper use of the machines. Ask your doctor for advice on using public blood pressure machines.
Causes
There are two types of high blood pressure.
Primary (essential) hypertension
For most adults, there's no identifiable cause of high blood pressure. This type of high blood pressure, called primary (essential) hypertension, tends to develop gradually over many years.
Secondary hypertension
Some people have high blood pressure caused by an underlying condition. This type of high blood pressure, called secondary hypertension, tends to appear suddenly and cause higher blood pressure than does primary hypertension. Various conditions and medications can lead to secondary hypertension, including:
- Obstructive sleep apnea
- Kidney problems
- Adrenal gland tumors
- Thyroid problems
- Certain defects in blood vessels you're born with (congenital)
- Certain medications, such as birth control pills, cold remedies, decongestants, over-the-counter pain relievers and some prescription drugs
- Illegal drugs, such as cocaine and amphetamines
- Alcohol abuse or chronic alcohol use
Risk factors
High blood pressure has many risk factors, including:
- Age. The risk of high blood pressure increases as you age. Through early middle age, or about age 45, high blood pressure is more common in men. Women are more likely to develop high blood pressure after age 65.
- Race. High blood pressure is particularly common among blacks, often developing at an earlier age than it does in whites. Serious complications, such as stroke, heart attack and kidney failure, also are more common in blacks.
- Family history. High blood pressure tends to run in families.
- Being overweight or obese. The more you weigh the more blood you need to supply oxygen and nutrients to your tissues. As the volume of blood circulated through your blood vessels increases, so does the pressure on your artery walls.
- Not being physically active. People who are inactive tend to have higher heart rates. The higher your heart rate, the harder your heart must work with each contraction and the stronger the force on your arteries. Lack of physical activity also increases the risk of being overweight.
- Using tobacco. Not only does smoking or chewing tobacco immediately raise your blood pressure temporarily, but the chemicals in tobacco can damage the lining of your artery walls. This can cause your arteries to narrow, increasing your blood pressure. Secondhand smoke also can increase your blood pressure.
- Too much salt (sodium) in your diet. Too much sodium in your diet can cause your body to retain fluid, which increases blood pressure.
- Too little potassium in your diet. Potassium helps balance the amount of sodium in your cells. If you don't get enough potassium in your diet or retain enough potassium, you may accumulate too much sodium in your blood.
- Too little vitamin D in your diet. It's uncertain if having too little vitamin D in your diet can lead to high blood pressure. Vitamin D may affect an enzyme produced by your kidneys that affects your blood pressure.
- Drinking too much alcohol. Over time, heavy drinking can damage your heart. Having more than two drinks a day for men and more than one drink a day for women may affect your blood pressure.
If you drink alcohol, do so in moderation. For healthy adults, that means up to one drink a day for women of all ages and men older than age 65, and up to two drinks a day for men age 65 and younger. One drink equals 12 ounces of beer, 5 ounces of wine or 1.5 ounces of 80-proof liquor. - Stress. High levels of stress can lead to a temporary increase in blood pressure. If you try to relax by eating more, using tobacco or drinking alcohol, you may only increase problems with high blood pressure.
- Certain chronic conditions. Certain chronic conditions also may increase your risk of high blood pressure, such as kidney disease, diabetes and sleep apnea.
Sometimes pregnancy contributes to high blood pressure, as well.
Although high blood pressure is most common in adults, children may be at risk, too. For some children, high blood pressure is caused by problems with the kidneys or heart. But for a growing number of kids, poor lifestyle habits, such as an unhealthy diet, obesity and lack of exercise, contribute to high blood pressure.
Complications
The excessive pressure on your artery walls caused by high blood pressure can damage your blood vessels, as well as organs in your body. The higher your blood pressure and the longer it goes uncontrolled, the greater the damage.
Uncontrolled high blood pressure can lead to:
- Heart attack or stroke. High blood pressure can cause hardening and thickening of the arteries (atherosclerosis), which can lead to a heart attack, stroke or other complications.
- Aneurysm. Increased blood pressure can cause your blood vessels to weaken and bulge, forming an aneurysm. If an aneurysm ruptures, it can be life-threatening.
- Heart failure. To pump blood against the higher pressure in your vessels, your heart muscle thickens. Eventually, the thickened muscle may have a hard time pumping enough blood to meet your body's needs, which can lead to heart failure.
- Weakened and narrowed blood vessels in your kidneys. This can prevent these organs from functioning normally.
- Thickened, narrowed or torn blood vessels in the eyes. This can result in vision loss.
- Metabolic syndrome. This syndrome is a cluster of disorders of your body's metabolism, including increased waist circumference; high triglycerides; low high-density lipoprotein (HDL) cholesterol, the "good" cholesterol; high blood pressure; and high insulin levels. These conditions make you more likely to develop diabetes, heart disease and stroke.
- Trouble with memory or understanding. Uncontrolled high blood pressure may also affect your ability to think, remember and learn. Trouble with memory or understanding concepts is more common in people with high blood pressure.
-
Interstitial lung disease
Interstitial (in-tur-STISH-ul) lung disease describes a large group of disorders, most of which cause progressive scarring of lung tissue. The scarring associated with interstitial lung disease eventually affects your ability to breathe and get enough oxygen into your bloodstream.
Interstitial lung disease can be caused by long-term exposure to hazardous materials, such as asbestos. Some types of autoimmune diseases, such as rheumatoid arthritis, also can cause interstitial lung disease. In some cases, however, the causes remain unknown.
Once lung scarring occurs, it's generally irreversible. Medications may slow the damage of interstitial lung disease, but many people never regain full use of their lungs. Lung transplant is an option for some people who have interstitial lung disease.
Symptoms
The primary signs and symptoms of interstitial lung disease are: Shortness of breath at rest or aggravated by exertion Dry cough When to see a doctor By the time symptoms appear, irreversible lung damage has often already occurred. Nevertheless, it's important to see your doctor at the first sign of breathing problems. Many conditions other than interstitial lung disease can affect your lungs, and getting an early and accurate diagnosis is important for proper treatment.
Causes
Bronchioles and alveoli in the lungs Bronchioles and alveoli in the lungs Interstitial lung disease seems to occur when an injury to your lungs triggers an abnormal healing response. Ordinarily, your body generates just the right amount of tissue to repair damage. But in interstitial lung disease, the repair process goes awry and the tissue around the air sacs (alveoli) becomes scarred and thickened. This makes it more difficult for oxygen to pass into your bloodstream.
Interstitial lung disease can be triggered by many different things — including airborne toxins in the workplace, drugs and some types of medical treatments. In most cases, the causes are unknown.
Occupational and environmental factors
Long-term exposure to a number of toxins and pollutants can damage your lungs. These may include:
- Silica dust
- Asbestos fibers
- Grain dust
- Bird and animal droppings
- Radiation treatments
- Indoor hot tubs
Some people who receive radiation therapy for lung or breast cancer show signs of lung damage months or sometimes years after the initial treatment.
Medications
Many drugs can damage your lungs, especially:
- Chemotherapy drugs. Drugs designed to kill cancer cells, such as methotrexate (Otrexup, Trexall, others) and cyclophosphamide, can also damage lung tissue.
- Heart medications. Some drugs used to treat irregular heartbeats, such as amiodarone (Nexterone, Pacerone) or propranolol (Inderal, Innopran), may harm lung tissue.
- Some antibiotics. Nitrofurantoin (Macrobid, Macrodantin, others) and ethambutol (Myambutol) can cause lung damage.
- Anti-inflammatory drugs. Certain anti-inflammatory drugs, such as rituximab (Rituxan) or sulfasalazine (Azulfidine), can cause lung damage.
Medical conditions
Lung damage can also result from autoimmune diseases such as:
- Rheumatoid arthritis
- Scleroderma
- Dermatomyositis and polymyositis
- Mixed connective tissue disease
- Sjogren's syndrome
- Sarcoidosis
The list of substances and conditions that can lead to interstitial lung disease is long. Even so, in some cases, the causes are never found. Disorders without a known cause are grouped together under the label of idiopathic interstitial pneumonias, the most common and deadly of which is idiopathic pulmonary fibrosis.
Risk factors
Factors that may make you more susceptible to interstitial lung disease include:
- Age. Interstitial lung disease is much more likely to affect adults, although infants and children sometimes develop the disorder.
- Exposure to occupational and environmental toxins. If you work in mining, farming or construction or for any reason are exposed to pollutants known to damage your lungs, your risk of interstitial lung disease is increased.
- Gastroesophageal reflux disease. If you have uncontrolled acid reflux or indigestion, you may be at increased risk of interstitial lung disease.
- Smoking. Some forms of interstitial lung disease are more likely to occur in people with a history of smoking, and active smoking may make the condition worse, especially if there is associated emphysema.
- Radiation and chemotherapy. Having radiation treatments to your chest or using some chemotherapy drugs makes it more likely that you'll develop lung disease.
Complications
Interstitial lung disease can lead to a series of life-threatening complications, including:
- High blood pressure in your lungs (pulmonary hypertension). Unlike systemic high blood pressure, this condition affects only the arteries in your lungs. It begins when scar tissue or low oxygen levels restrict the smallest blood vessels, limiting blood flow in your lungs. This in turn raises pressure within the pulmonary arteries. Pulmonary hypertension is a serious illness that becomes progressively worse.
- Right-sided heart failure (cor pulmonale). This serious condition occurs when your heart's lower right chamber (right ventricle) — which is less muscular than the left — has to pump harder than usual to move blood through obstructed pulmonary arteries. Eventually the right ventricle fails from the extra strain. This is often a consequence of pulmonary hypertension.
- Respiratory failure. In the end stage of chronic interstitial lung disease, respiratory failure occurs when severely low blood oxygen levels along with rising pressures in the pulmonary arteries and the right ventricle cause heart failure.
-
Lung Cancer
Lung cancer is a type of cancer that begins in the lungs. Your lungs are two spongy organs in your chest that take in oxygen when you inhale and release carbon dioxide when you exhale.
Lung cancer is the leading cause of cancer deaths in the United States, among both men and women. Lung cancer claims more lives each year than do colon, prostate, ovarian and breast cancers combined.
People who smoke have the greatest risk of lung cancer, though lung cancer can also occur in people who have never smoked. The risk of lung cancer increases with the length of time and number of cigarettes you've smoked. If you quit smoking, even after smoking for many years, you can significantly reduce your chances of developing lung cancer.
Symptoms
Lung cancer typically doesn't cause signs and symptoms in its earliest stages. Signs and symptoms of lung cancer typically occur only when the disease is advanced.
Signs and symptoms of lung cancer may include:
- A new cough that doesn't go away
- Coughing up blood, even a small amount
- Shortness of breath
- Chest pain
- Hoarseness
- Losing weight without trying
- Bone pain
- Headache
When to see a doctor
Make an appointment with your doctor if you have any persistent signs or symptoms that worry you.
If you smoke and have been unable to quit, make an appointment with your doctor. Your doctor can recommend strategies for quitting smoking, such as counseling, medications and nicotine replacement products.
Causes
Smoking causes the majority of lung cancers — both in smokers and in people exposed to secondhand smoke. But lung cancer also occurs in people who never smoked and in those who never had prolonged exposure to secondhand smoke. In these cases, there may be no clear cause of lung cancer.
How smoking causes lung cancer
Doctors believe smoking causes lung cancer by damaging the cells that line the lungs. When you inhale cigarette smoke, which is full of cancer-causing substances (carcinogens), changes in the lung tissue begin almost immediately.
At first your body may be able to repair this damage. But with each repeated exposure, normal cells that line your lungs are increasingly damaged. Over time, the damage causes cells to act abnormally and eventually cancer may develop.
Types of lung cancer
Doctors divide lung cancer into two major types based on the appearance of lung cancer cells under the microscope. Your doctor makes treatment decisions based on which major type of lung cancer you have.
The two general types of lung cancer include:
- Small cell lung cancer. Small cell lung cancer occurs almost exclusively in heavy smokers and is less common than non-small cell lung cancer.
- Non-small cell lung cancer. Non-small cell lung cancer is an umbrella term for several types of lung cancers that behave in a similar way. Non-small cell lung cancers include squamous cell carcinoma, adenocarcinoma and large cell carcinoma.
Risk factors
A number of factors may increase your risk of lung cancer. Some risk factors can be controlled, for instance, by quitting smoking. And other factors can't be controlled, such as your family history.
Risk factors for lung cancer include:
- Smoking. Your risk of lung cancer increases with the number of cigarettes you smoke each day and the number of years you have smoked. Quitting at any age can significantly lower your risk of developing lung cancer.
- Exposure to secondhand smoke. Even if you don't smoke, your risk of lung cancer increases if you're exposed to secondhand smoke.
- Exposure to radon gas. Radon is produced by the natural breakdown of uranium in soil, rock and water that eventually becomes part of the air you breathe. Unsafe levels of radon can accumulate in any building, including homes.
- Exposure to asbestos and other carcinogens. Workplace exposure to asbestos and other substances known to cause cancer — such as arsenic, chromium and nickel — also can increase your risk of developing lung cancer, especially if you're a smoker.
- Family history of lung cancer. People with a parent, sibling or child with lung cancer have an increased risk of the disease.
Complications
Lung cancer can cause complications, such as:
- Shortness of breath. People with lung cancer can experience shortness of breath if cancer grows to block the major airways. Lung cancer can also cause fluid to accumulate around the lungs, making it harder for the affected lung to expand fully when you inhale.
- Coughing up blood. Lung cancer can cause bleeding in the airway, which can cause you to cough up blood (hemoptysis). Sometimes bleeding can become severe. Treatments are available to control bleeding.
- Pain. Advanced lung cancer that spreads to the lining of a lung or to another area of the body, such as a bone, can cause pain. Tell your doctor if you experience pain, as many treatments are available to control pain.
- Fluid in the chest (pleural effusion). Lung cancer can cause fluid to accumulate in the space that surrounds the affected lung in the chest cavity (pleural space).
Fluid accumulating in the chest can cause shortness of breath. Treatments are available to drain the fluid from your chest and reduce the risk that pleural effusion will occur again. - Cancer that spreads to other parts of the body (metastasis). Lung cancer often spreads (metastasizes) to other parts of the body, such as the brain and the bones.
Cancer that spreads can cause pain, nausea, headaches, or other signs and symptoms depending on what organ is affected. Once lung cancer has spread beyond the lungs, it's generally not curable. Treatments are available to decrease signs and symptoms and to help you live longer.
Prevention
There's no sure way to prevent lung cancer, but you can reduce your risk if you:
- Don't smoke. If you've never smoked, don't start. Talk to your children about not smoking so that they can understand how to avoid this major risk factor for lung cancer. Begin conversations about the dangers of smoking with your children early so that they know how to react to peer pressure.
- Stop smoking. Stop smoking now. Quitting reduces your risk of lung cancer, even if you've smoked for years. Talk to your doctor about strategies and stop-smoking aids that can help you quit. Options include nicotine replacement products, medications and support groups.
- Avoid secondhand smoke. If you live or work with a smoker, urge him or her to quit. At the very least, ask him or her to smoke outside. Avoid areas where people smoke, such as bars and restaurants, and seek out smoke-free options.
- Test your home for radon. Have the radon levels in your home checked, especially if you live in an area where radon is known to be a problem. High radon levels can be remedied to make your home safer. For information on radon testing, contact your local department of public health or a local chapter of the American Lung Association.
- Avoid carcinogens at work. Take precautions to protect yourself from exposure to toxic chemicals at work. Follow your employer's precautions. For instance, if you're given a face mask for protection, always wear it. Ask your doctor what more you can do to protect yourself at work. Your risk of lung damage from workplace carcinogens increases if you smoke.
- Eat a diet full of fruits and vegetables. Choose a healthy diet with a variety of fruits and vegetables. Food sources of vitamins and nutrients are best. Avoid taking large doses of vitamins in pill form, as they may be harmful. For instance, researchers hoping to reduce the risk of lung cancer in heavy smokers gave them beta carotene supplements. Results showed the supplements actually increased the risk of cancer in smokers.
- Exercise most days of the week. If you don't exercise regularly, start out slowly. Try to exercise most days of the week.
-
Pneumonia
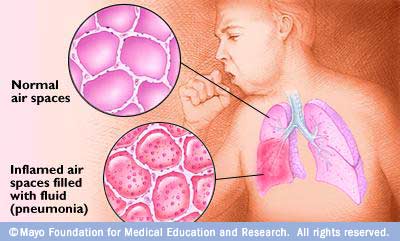 Pneumonia is an infection that inflames the air sacs in one or both lungs. The air sacs may fill with fluid or pus (purulent material), causing cough with phlegm or pus, fever, chills, and difficulty breathing. A variety of organisms, including bacteria, viruses and fungi, can cause pneumonia.
Pneumonia is an infection that inflames the air sacs in one or both lungs. The air sacs may fill with fluid or pus (purulent material), causing cough with phlegm or pus, fever, chills, and difficulty breathing. A variety of organisms, including bacteria, viruses and fungi, can cause pneumonia.
Pneumonia can range in seriousness from mild to life-threatening. It is most serious for infants and young children, people older than age 65, and people with health problems or weakened immune systems.
Symptoms
The signs and symptoms of pneumonia vary from mild to severe, depending on factors such as the type of germ causing the infection, and your age and overall health. Mild signs and symptoms often are similar to those of a cold or flu, but they last longer.
Signs and symptoms of pneumonia may include:
- Chest pain when you breathe or cough
- Confusion or changes in mental awareness (in adults age 65 and older)
- Cough, which may produce phlegm
- Fatigue
- Fever, sweating and shaking chills
- Lower than normal body temperature (in adults older than age 65 and people with weak immune systems)
- Nausea, vomiting or diarrhea
- Shortness of breath
Newborns and infants may not show any sign of the infection. Or they may vomit, have a fever and cough, appear restless or tired and without energy, or have difficulty breathing and eating.
When to see a doctor
See your doctor if you have difficulty breathing, chest pain, persistent fever of 102 F (39 C) or higher, or persistent cough, especially if you're coughing up pus.
It's especially important that people in these high-risk groups see a doctor:
- Adults older than age 65
- Children younger than age 2 with signs and symptoms
- People with an underlying health condition or weakened immune system
- People receiving chemotherapy or taking medication that suppresses the immune system
For some older adults and people with heart failure or chronic lung problems, pneumonia can quickly become a life-threatening condition.
Causes
Many germs can cause pneumonia. The most common are bacteria and viruses in the air we breathe. Your body usually prevents these germs from infecting your lungs. But sometimes these germs can overpower your immune system, even if your health is generally good.
Pneumonia is classified according to the types of germs that cause it and where you got the infection.
Community-acquired pneumonia
Community-acquired pneumonia is the most common type of pneumonia. It occurs outside of hospitals or other healthcare facilities. It may be caused by:
- Bacteria. The most common cause of bacterial pneumonia in the U.S. is Streptococcus pneumoniae. This type of pneumonia can occur on its own or after you've had a cold or the flu. It may affect one part (lobe) of the lung, a condition called lobar pneumonia.
- Bacteria-like organisms. Mycoplasma pneumoniae also can cause pneumonia. It typically produces milder symptoms than do other types of pneumonia. Walking pneumonia is an informal name given to this type of pneumonia, which typically isn't severe enough to require bed rest.
- Fungi. This type of pneumonia is most common in people with chronic health problems or weakened immune systems, and in people who have inhaled large doses of the organisms. The fungi that cause it can be found in soil or bird droppings and vary depending upon geographic location.
- Viruses. Some of the viruses that cause colds and the flu can cause pneumonia. Viruses are the most common cause of pneumonia in children younger than 5 years. Viral pneumonia is usually mild. But in some cases it can become very serious.
Hospital-acquired pneumonia
Some people catch pneumonia during a hospital stay for another illness. Hospital-acquired pneumonia can be serious because the bacteria causing it may be more resistant to antibiotics and because the people who get it are already sick. People who are on breathing machines (ventilators), often used in intensive care units, are at higher risk of this type of pneumonia.
Healthcare-acquired pneumonia
Healthcare-acquired pneumonia is a bacterial infection that occurs in people who live in long-term care facilities or who receive care in outpatient clinics, including kidney dialysis centers. Like hospital-acquired pneumonia, healthcare-acquired pneumonia can be caused by bacteria that are more resistant to antibiotics.
Aspiration pneumonia
Aspiration pneumonia occurs when you inhale food, drink, vomit or saliva into your lungs. Aspiration is more likely if something disturbs your normal gag reflex, such as a brain injury or swallowing problem, or excessive use of alcohol or drugs.
Risk factors
Pneumonia can affect anyone. But the two age groups at highest risk are:
- Children who are 2 years old or younger
- People who are age 65 or older
Other risk factors include:
- Being hospitalized. You're at greater risk of pneumonia if you're in a hospital intensive care unit, especially if you're on a machine that helps you breathe (a ventilator).
- Chronic disease. You're more likely to get pneumonia if you have asthma, chronic obstructive pulmonary disease (COPD) or heart disease.
- Smoking. Smoking damages your body's natural defenses against the bacteria and viruses that cause pneumonia.
- Weakened or suppressed immune system. People who have HIV/AIDS, who've had an organ transplant, or who receive chemotherapy or long-term steroids are at risk.
Complications
Even with treatment, some people with pneumonia, especially those in high-risk groups, may experience complications, including:
- Bacteria in the bloodstream (bacteremia). Bacteria that enter the bloodstream from your lungs can spread the infection to other organs, potentially causing organ failure.
- Difficulty breathing. If your pneumonia is severe or you have chronic underlying lung diseases, you may have trouble breathing in enough oxygen. You may need to be hospitalized and use a breathing machine (ventilator) while your lung heals.
- Fluid accumulation around the lungs (pleural effusion). Pneumonia may cause fluid to build up in the thin space between layers of tissue that line the lungs and chest cavity (pleura). If the fluid becomes infected, you may need to have it drained through a chest tube or removed with surgery.
- Lung abscess. An abscess occurs if pus forms in a cavity in the lung. An abscess is usually treated with antibiotics. Sometimes, surgery or drainage with a long needle or tube placed into the abscess is needed to remove the pus.
Prevention
To help prevent pneumonia:
- Get vaccinated. Vaccines are available to prevent some types of pneumonia and the flu. Talk with your doctor about getting these shots. The vaccination guidelines have changed over time so make sure to review your vaccination status with your doctor even if you recall previously receiving a pneumonia vaccine.
- Make sure children get vaccinated. Doctors recommend a different pneumonia vaccine for children younger than age 2 and for children ages 2 to 5 years who are at particular risk of pneumococcal disease. Children who attend a group child care center should also get the vaccine. Doctors also recommend flu shots for children older than 6 months.
- Practice good hygiene. To protect yourself against respiratory infections that sometimes lead to pneumonia, wash your hands regularly or use an alcohol-based hand sanitizer.
- Don't smoke. Smoking damages your lungs' natural defenses against respiratory infections.
- Keep your immune system strong. Get enough sleep, exercise regularly and eat a healthy diet.
-
Pulmonary Fibrosis
Pulmonary fibrosis is a lung disease that occurs when lung tissue becomes damaged and scarred. This thickened, stiff tissue makes it more difficult for your lungs to work properly. As pulmonary fibrosis worsens, you become progressively more short of breath.
The scarring associated with pulmonary fibrosis can be caused by a multitude of factors. But in most cases, doctors can't pinpoint what's causing the problem. When a cause can't be found, the condition is termed idiopathic pulmonary fibrosis.
The lung damage caused by pulmonary fibrosis can't be repaired, but medications and therapies can sometimes help ease symptoms and improve quality of life. For some people, a lung transplant might be appropriate.
Symptoms
Signs and symptoms of pulmonary fibrosis may include:
- Shortness of breath (dyspnea)
- A dry cough
- Fatigue
- Unexplained weight loss
- Aching muscles and joints
- Widening and rounding of the tips of the fingers or toes (clubbing)
The course of pulmonary fibrosis — and the severity of symptoms — can vary considerably from person to person. Some people become ill very quickly with severe disease. Others have moderate symptoms that worsen more slowly, over months or years.
Some people may experience a rapid worsening of their symptoms (acute exacerbation), such as severe shortness of breath, that may last for several days to weeks. People who have acute exacerbations may be placed on a mechanical ventilator. Doctors may also prescribe antibiotics, corticosteroid medications or other medications to treat an acute exacerbation.
Causes
Pulmonary fibrosis scars and thickens the tissue around and between the air sacs (alveoli) in your lungs. This makes it more difficult for oxygen to pass into your bloodstream. The damage can be caused by many different factors — including long-term exposure to certain toxins, certain medical conditions, radiation therapy and some medications.
Occupational and environmental factors
Long-term exposure to a number of toxins and pollutants can damage your lungs. These include:
- Silica dust
- Asbestos fibers
- Hard metal dusts
- Coal dust
- Grain dust
- Bird and animal droppings
Radiation treatments
Some people who receive radiation therapy for lung or breast cancer show signs of lung damage months or sometimes years after the initial treatment. The severity of the damage may depend on:
- How much of the lung was exposed to radiation
- The total amount of radiation administered
- Whether chemotherapy also was used
- The presence of underlying lung disease
Medications
Many drugs can damage your lungs, especially medications such as:
- Chemotherapy drugs. Drugs designed to kill cancer cells, such as methotrexate (Trexall, Otrexup, others) and cyclophosphamide, can also damage lung tissue.
- Heart medications. Some drugs used to treat irregular heartbeats, such as amiodarone (Cordarone, Nexterone, Pacerone), may harm lung tissue.
- Some antibiotics. Antibiotics such as nitrofurantoin (Macrobid, Macrodantin, others) or ethambutol can cause lung damage.
- Anti-inflammatory drugs. Certain anti-inflammatory drugs such as rituximab (Rituxan) or sulfasalazine (Azulfidine) can cause lung damage.
Medical conditions
Lung damage can also result from a number of conditions, including:
- Dermatomyositis
- Polymyositis
- Mixed connective tissue disease
- Systemic lupus erythematosus
- Rheumatoid arthritis
- Sarcoidosis
- Scleroderma
- Pneumonia
Many substances and conditions can lead to pulmonary fibrosis. Even so, in most cases, the cause is never found. Pulmonary fibrosis with no known cause is called idiopathic pulmonary fibrosis.
Researchers have several theories about what might trigger idiopathic pulmonary fibrosis, including viruses and exposure to tobacco smoke. Also, some forms of idiopathic pulmonary fibrosis run in families, and heredity may play a role in idiopathic pulmonary fibrosis.
Many people with idiopathic pulmonary fibrosis may also have gastroesophageal reflux disease (GERD) — a condition that occurs when acid from your stomach flows back into your esophagus. Ongoing research is evaluating if GERD may be a risk factor for idiopathic pulmonary fibrosis, or if GERD may lead to a more rapid progression of the condition. However, more research is needed to determine the association between idiopathic pulmonary fibrosis and GERD.
Risk factors
Factors that make you more susceptible to pulmonary fibrosis include:
- Age. Although pulmonary fibrosis has been diagnosed in children and infants, the disorder is much more likely to affect middle-aged and older adults.
- Sex. Idiopathic pulmonary fibrosis is more likely to affect men than women.
- Smoking. Far more smokers and former smokers develop pulmonary fibrosis than do people who have never smoked. Pulmonary fibrosis can occur in patients with emphysema.
- Certain occupations. You have an increased risk of developing pulmonary fibrosis if you work in mining, farming or construction or if you're exposed to pollutants known to damage your lungs.
- Cancer treatments. Having radiation treatments to your chest or using certain chemotherapy drugs can increase your risk of pulmonary fibrosis.
- Genetic factors. Some types of pulmonary fibrosis run in families, and genetic factors may be a component.
Complications
Complications of pulmonary fibrosis may include:
- High blood pressure in your lungs (pulmonary hypertension). Unlike systemic high blood pressure, this condition affects only the arteries in your lungs. It begins when the smallest arteries and capillaries are compressed by scar tissue, causing increased resistance to blood flow in your lungs.
This in turn raises pressure within the pulmonary arteries and the lower right heart chamber (right ventricle). Some forms of pulmonary hypertension are serious illnesses that become progressively worse and are sometimes fatal. - Right-sided heart failure (cor pulmonale). This serious condition occurs when your heart's lower right chamber (ventricle) has to pump harder than usual to move blood through partially blocked pulmonary arteries.
- Respiratory failure. This is often the last stage of chronic lung disease. It occurs when blood oxygen levels fall dangerously low.
- Lung cancer. Long-standing pulmonary fibrosis also increases your risk of developing lung cancer.
- Lung complications. As pulmonary fibrosis progresses, it may lead to complications such as blood clots in the lungs, a collapsed lung or lung infections.
-
sleep and sleep apnea
Sleep apnea is a potentially serious sleep disorder in which breathing repeatedly stops and starts. You may have sleep apnea if you snore loudly, and you feel tired even after a full night's sleep.
The main types of sleep apnea are:
- Obstructive sleep apnea, the more common form that occurs when throat muscles relax.
- Central sleep apnea, which occurs when your brain doesn't send proper signals to the muscles that control breathing.
- Complex sleep apnea syndrome, also known as treatment-emergent central sleep apnea, occurs when someone has both obstructive sleep apnea and central sleep apnea.
If you think you might have any form of sleep apnea, see your doctor. Treatment can ease your symptoms and may help prevent heart problems and other complications.
Symptoms
The signs and symptoms of obstructive and central sleep apneas overlap, sometimes making the type of sleep apnea more difficult to determine. The most common signs and symptoms of obstructive and central sleep apneas include:
- Loud snoring, which is usually more prominent in obstructive sleep apnea
- Episodes of breathing cessation during sleep witnessed by another person
- Abrupt awakenings accompanied by shortness of breath, which more likely indicates central sleep apnea
- Awakening with a dry mouth or sore throat
- Morning headache
- Difficulty staying asleep (insomnia)
- Excessive daytime sleepiness (hypersomnia)
- Attention problems
- Irritability
When to see a doctor
Consult a medical professional if you experience, or if your partner notices, the following:
- Snoring loud enough to disturb the sleep of others or yourself
- Shortness of breath, gasping for air or choking that awakens you from sleep
- Intermittent pauses in your breathing during sleep
- Excessive daytime drowsiness, which may cause you to fall asleep while you're working, watching television or even driving
Many people don't think of snoring as a sign of something potentially serious, and not everyone who has sleep apnea snores. But be sure to talk to your doctor if you experience loud snoring, especially snoring that's punctuated by periods of silence.
Ask your doctor about any sleep problem that leaves you chronically fatigued, sleepy and irritable. Excessive daytime drowsiness (hypersomnia) may be due to sleep apnea or to other disorders, such as narcolepsy.
Causes
Causes of obstructive sleep apnea
Obstructive sleep apnea occurs when the muscles in the back of your throat relax. These muscles support the soft palate, the triangular piece of tissue hanging from the soft palate (uvula), the tonsils, the side walls of the throat and the tongue.
When the muscles relax, your airway narrows or closes as you breathe in, and you can't get an adequate breath in. This may lower the level of oxygen in your blood.
Your brain senses this inability to breathe and briefly rouses you from sleep so that you can reopen your airway. This awakening is usually so brief that you don't remember it.
You may make a snorting, choking or gasping sound. This pattern can repeat itself five to 30 times or more each hour, all night long. These disruptions impair your ability to reach the desired deep, restful phases of sleep, and you'll probably feel sleepy during your waking hours.
People with obstructive sleep apnea may not be aware that their sleep was interrupted. In fact, some people with this type of sleep apnea think they sleep well all night.
Causes of central sleep apnea
Central sleep apnea is a less common form of sleep apnea that occurs when your brain fails to transmit signals to your breathing muscles. This means you make no effort to breathe for a short period of time. You may awaken with shortness of breath or have a difficult time getting to sleep or staying asleep.
Risk factors
Sleep apnea can affect anyone, even children. But certain factors increase your risk of sleep apnea:
Obstructive sleep apnea
- Excess weight. People who are obese have four times the risk of sleep apnea that people who are a normal weight people do. Fat deposits around your upper airway may obstruct your breathing. But not everyone who has sleep apnea is overweight.
- Neck circumference. People with thicker necks may have narrower airways. For men, the risk increases if neck circumference is 17 inches (43 centimeters) and larger. In women, the risk increases if neck circumference is 15 inches (38 centimeters) or more.
- A narrowed airway. You may have inherited a naturally narrow throat. Or, tonsils or adenoids may become enlarged and block the airway, particularly in children with sleep apnea.
- Being male. Men are twice as likely to have sleep apnea. However, women increase their risk if they're overweight, and their risk also appears to rise after menopause.
- Being older. Sleep apnea occurs significantly more often in older adults.
- Family history. If you have family members with sleep apnea, you may be at increased risk.
- Use of alcohol, sedatives or tranquilizers. These substances relax the muscles in your throat.
- Smoking. Smokers are three times more likely to have obstructive sleep apnea than are people who've never smoked. Smoking may increase the amount of inflammation and fluid retention in the upper airway. This risk likely drops after you quit smoking.
- Nasal congestion. If you have difficulty breathing through your nose — whether it's from an anatomical problem or allergies — you're more likely to develop obstructive sleep apnea.
Central sleep apnea
- Being older. Middle-aged and older people have a higher risk of central sleep apnea.
- Heart disorders. People with congestive heart failure are more at risk of central sleep apnea.
- Using narcotic pain medications. Opioid medications, especially long-acting ones such as methadone, increase the risk of central sleep apnea.
- Stroke. People who've had a stroke are more at risk of central sleep apnea or treatment-emergent central sleep apnea.
Complications
Sleep apnea is considered a serious medical condition. Complications may include:
- Daytime fatigue. The repeated awakenings associated with sleep apnea make normal, restorative sleep impossible. People with sleep apnea often experience severe daytime drowsiness, fatigue and irritability.
You may have difficulty concentrating and find yourself falling asleep at work, while watching TV or even when driving. People with sleep apnea have an increased risk of motor vehicle and workplace accidents.
You may also feel quick tempered, moody or depressed. Children and adolescents with sleep apnea may do poorly in school or have behavior problems. - High blood pressure or heart problems. Sudden drops in blood oxygen levels that occur during sleep apnea increase blood pressure and strain the cardiovascular system. If you have obstructive sleep apnea, your risk of high blood pressure (hypertension) is greater than if you don't.
Obstructive sleep apnea may increase the risk of recurrent heart attack, and abnormal heartbeats, such as atrial fibrillation. Obstructive sleep apnea also increases the risk of stroke. If there's underlying heart disease, these multiple episodes of low blood oxygen (hypoxia or hypoxemia) can lead to sudden death from an irregular heartbeat. - Type 2 diabetes. People with sleep apnea are more likely to develop insulin resistance and type 2 diabetes compared with people without the sleep disorder.
- Metabolic syndrome. This disorder is a collection of other risk factors linked to a higher risk of heart disease. The conditions that make up metabolic syndrome include high blood pressure, abnormal cholesterol, high blood sugar and an increased waist circumference.
- Complications with medications and surgery. Obstructive sleep apnea is also a concern with certain medications and general anesthesia. People with sleep apnea may be more likely to experience complications following major surgery because they're prone to breathing problems, especially when sedated and lying on their backs. Before you have surgery, tell your doctor that you have sleep apnea and how it's treated.
- Liver problems. People with sleep apnea are more likely to have abnormal results on liver function tests, and their livers are more likely to show signs of scarring. This is a condition known as nonalcoholic fatty liver disease.
- Sleep-deprived partners. Loud snoring can keep those around you from getting good rest and eventually disrupt your relationships. It's not uncommon for a partner to go to another room, or even on another floor of the house, to be able to sleep. Many bed partners of people who snore may be sleep-deprived as well.
Learn about diagnosis and treatment.
To eliminate snoring and prevent sleep apnea, your doctor may recommend a device called a continuous positive airway pressure (CPAP) machine. A CPAP machine delivers just enough air pressure to a mask to keep your upper airway passages open, preventing snoring and sleep apnea.



