Recent Posts
Redefining liver health: Understanding steatotic liver disease

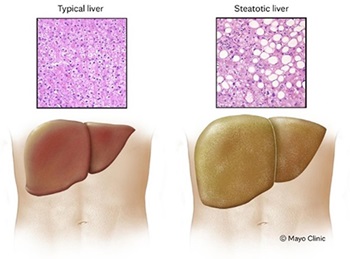
For many years, nonalcoholic fatty liver disease (NAFLD) has referred to a range of liver conditions that develop when too much fat is stored in the liver cells. It's the most common form of chronic liver disease, affecting 25–30% of the world's adult population, and is on the rise globally.
A shift is underway to change the name of fatty liver disease to steatotic liver disease (SLD). Why does the name change matter? The "nonalcoholic" reference doesn't accurately capture the cause of the disease, and "fatty" has a negative association.
Categories of SLD include:
- Metabolic dysfunction-associated steatotic liver disease (MASLD), formerly known as nonalcoholic fatty liver disease (NAFLD)
- MASLD and increased alcohol intake (MetALD)
- Alcohol-related liver disease (ALD)
- Specific etiology SLD, which includes drug-induced liver injury and liver disease from celiac disease or malnutrition
- Cryptogenic SLD, which is liver disease with an uncertain origin
Some people can develop an aggressive form of MADLD called metabolic-associated steatohepatitis, or MASH. The primary concern with MASH is that liver inflammation can progress to advanced scarring, called fibrosis. If inflammation is ongoing, the fibrosis can spread and take up more liver tissue.
Causes of liver disease
Medical professionals have yet to figure out exactly why fat accumulates in the liver of some people.
Certain factors linked to the condition include:
- Genetics
- Obesity or being overweight
- High blood sugar, called hyperglycemia, which can indicate prediabetes or Type 2 diabetes
- High levels of fats in the blood, particularly triglycerides
These factors may lead to the accumulation of fat in the liver, which can cause chronic liver disease over time.
Symptoms of liver disease
People with early MASLD often have no symptoms of the disease. General symptoms may include fatigue, not feeling well or pain in the right upper belly area.
When liver disease has progressed to advanced fibrosis or severe scarring of the liver, called cirrhosis, possible symptoms include:
- Abdominal swelling from ascites, which is fluid in the belly
- Enlarged spleen
- Gastrointestinal bleeding
- Itchy skin
- Mental confusion
- Shortness of breath
- Swelling in the legs
- Yellowing of the eyes and skin, or jaundice
Contact your healthcare professional to discuss your risk factors for liver disease and have any symptoms evaluated.
Getting screened for liver disease
Because there are no obvious signs or symptoms of liver disease in its early stages, it can develop and go undiagnosed for many years. Screening and early diagnosis are crucial for identifying and managing the condition.
Several noninvasive screening methods are available, including bloodwork and imaging tests like abdominal ultrasound and transient elastography. Your primary care provider, endocrinologist, cardiologist or gastroenterologist can order these screenings.
If a member of your care team determines that you are at increased risk of steatotic liver disease or have advanced fibrosis or cirrhosis, they will likely refer you to a gastroenterologist or hepatologist for evaluation and treatment.
Living with liver disease
You can prevent, slow or improve steatotic liver disease by taking actions that help control the disease. If you're overweight or obese, the first step should be weight loss, combined with a healthy diet and exercise.
Actions you can take include:
- Control your diabetes.
If you have prediabetes or diabetes, ask your healthcare team about being screened for steatotic liver disease. Liver disease affects up to 70% of people with Type 2 diabetes, according to the American Diabetes Association. If you have diabetes, monitor your blood sugar and take your medications as directed by your healthcare team to manage your condition. - Eat a healthy diet.
Your meal plan should include fruits, vegetables, lean proteins and whole grains. Avoid sugary drinks and pay attention to portion sizes. Interestingly, drinking at least three cups of coffee daily is associated with less-advanced liver disease. - Exercise and look for ways to be active.
Whether or not you're trying to lose weight, being active is good for you. Try to get at least 30 minutes of exercise most days of the week. If you haven't been exercising regularly, talk with your healthcare team first and then slowly start a routine. - Go to your medical appointments.
Liver health is crucial. If you have liver disease, you may have a team of healthcare professionals in primary care, gastroenterology, endocrinology and cardiology working together to assess, manage and treat your condition. - Lose weight.
A healthy diet and exercise are effective methods to lose weight. Consider working with a registered dietitian to help evaluate your caloric needs to achieve weight loss. If you're overweight or obese, talk with your healthcare team about weight loss programs or bariatric surgery. - Lower your cholesterol.
If you have high cholesterol or triglycerides, medication, a plant-based diet and exercise can help keep your blood lipid levels at an average level. - Protect your liver.
Drinking alcohol can put extra stress on your liver. Limiting or avoiding alcohol is typically advised for people with liver disease. Those same steps also can prevent liver disease for people who haven't developed the condition. Follow the instructions on prescription medications and over-the-counter medications. Consult with your healthcare professional before taking herbal supplements. There's no approved or safe way to detoxify your liver, so avoid regimens claiming they can do it.
Next steps:
- Find a gastroenterologist near you.
- Learn more about liver disease.
- Read how cirrhosis affects your liver.
- Get prevention and self-care tips for your digestive system.
Victoria Louwagie is a physician assistant in Gastroenterology in Mankato, Minnesota.