Screenings, awareness help prevent cervical cancer

Cases of cervical cancer, which once was the leading cause of deaths in women, have decreased in recent years. However, the Centers for Disease Control and Prevention notes that more than 12,700 cases of cervical cancer were diagnosed and more than 4,100 women died from the disease in 2018. These figures show that cervical cancer remains a major threat to the health and well-being of women.
What is cervical cancer?
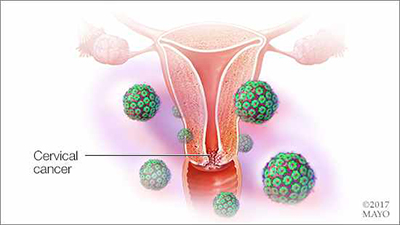
Cervical cancer begins when healthy cells in the cervix, the lower part of the uterus that connects to the vagina, develop mutations in their DNA. A cell's DNA contains instructions that tell the cell what to do. Healthy cells grow and multiply at a set rate, eventually dying at a set time. The mutations tell the cells to grow and multiply out of control, and they don't die. The accumulating abnormal cells form a mass, or tumor. Cancer cells invade nearby tissues and can break off from a tumor to spread, or metastasize, elsewhere in the body.
The most common types are squamous cell carcinoma, which occurs in squamous cells, which line the outer part of the cervix, and adenocarcinoma, which develops in glandular cells in the cervical canal.
Many strains of the human papillomavirus (HPV), a sexually transmitted infection, contribute to the growth of cervical cancer cells. Many women's immune systems combat HPV, preventing the virus from causing cancer. Yet, some women are more susceptible to cervical cancer, as HPV lives in their bodies for years and aids in the emergence of cancer cells.
Are symptoms of cervical cancer obvious?
Symptoms of cervical cancer are not obvious. Most women with cervical cancer don't experience any signs in early stages.
As the disease progresses, symptoms could include:
- Vaginal bleeding after intercourse, between periods or after menopause
- Watery, bloody vaginal discharge that may be heavy and have a foul odor
- Pelvic pain or lower back pain
Talk to your primary care provider as soon as possible if you have worrisome symptoms.
What elevates the risk of cervical cancer?
Risk factors for cervical cancer include:
- Multiple sexual partners
- Sexual activity at a young age
- Other sexually transmitted infections
- Weak immune system
- Smoking
How can you prevent cervical cancer?
The most effective ways to reduce cervical cancer risk include:
- Getting vaccinated against HPV.
The two-dose HPV vaccine is recommended for all 11- and 12-year-olds. This is the best age to receive the vaccine to protect against the virus. Children as young as 9 can receive the vaccine. Teens and young adults, from ages 15 to 26, also can receive three doses of the vaccine. Some adults ages 27 to 45 might decide to get the HPV vaccine based on a conversation with their health care providers. - Having routine Pap tests.
Most health care experts recommend Pap tests, which detect precancerous conditions of the cervix, beginning at age 21. Read the updated recommendation for Pap tests. - Practicing safe sex.
Limiting sexual partners, using condoms and abstaining from sex at early ages helps limit risk. - Not smoking.
Don't smoke, or quit if you do. Smoking is linked to squamous cell cervical cancer.
Can cervical cancer be treated?
Cervical cancer can be treated. Treatment options are available depending on the stage of the disease, your health status and personal preferences. The earlier cervical cancer is detected, the more successful treatment tends to be. Common treatments include surgery, radiation, chemotherapy or a combination of these treatments.
After consulting with their health care team, some women may choose to have a hysterectomy, which is a removal of the uterus, to cure early stage cervical cancer and prevent recurrence. A hysterectomy makes it impossible to conceive a child in the future.
Through awareness and diligent health management, patients and health care providers can continue to reduce the instances of, and deaths from, cervical cancer.
Ruta Kirstein is an nurse practitioner in Oncology in Eau Claire and Menomonie, Wisconsin.