
Orthopedics & Orthopedic Surgery (Bones)
Foot & Ankle Care in Onalaska
If you're experiencing problems or pain with the skin, muscles, ligaments, nerves and bones of the foot and ankle, our comprehensive team of foot and ankle specialists can help you get back on your feet — pain free.
Our orthopedic providers will address injuries, such as fractures, sprains and strains. We'll also treat general aches and pains acquired through daily and recreational activities. We may try nonoperative techniques, such as physical therapy and braces. Surgery may be necessary for tendon repair, fracture care, reconstruction and arthroscopy, a procedure for diagnosing and treating joint problems.
Additionally, our team includes a podiatrist who can assist with common foot and ankle needs.
- Achilles tendon rupture
- Ankle arthritis:
- Broken foot
- Bunions
- Flat feet
Visit our Podiatry page for more information.
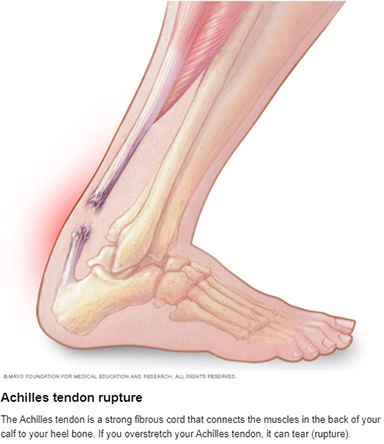
Achilles tendon rupture
 Achilles (uh-KILL-eez) tendon rupture is an injury that affects the back of your lower leg. It mainly occurs in people playing recreational sports, but it can happen to anyone.
Achilles (uh-KILL-eez) tendon rupture is an injury that affects the back of your lower leg. It mainly occurs in people playing recreational sports, but it can happen to anyone.
The Achilles tendon is a strong fibrous cord that connects the muscles in the back of your calf to your heel bone. If you overstretch your Achilles tendon, it can tear (rupture) completely or just partially.
If your Achilles tendon ruptures, you might hear a pop, followed by an immediate sharp pain in the back of your ankle and lower leg that is likely to affect your ability to walk properly. Surgery is often performed to repair the rupture. For many people, however, nonsurgical treatment works just as well.
Symptoms
Although it's possible to have no signs or symptoms with an Achilles tendon rupture, most people have:
- The feeling of having been kicked in the calf
- Pain, possibly severe, and swelling near the heel
- An inability to bend the foot downward or "push off" the injured leg when walking
- An inability to stand on the toes on the injured leg
- A popping or snapping sound when the injury occurs
When to see your doctor
Seek medical advice immediately if you hear a pop in your heel, especially if you can't walk properly afterward.
Causes
Your Achilles tendon helps you point your foot downward, rise on your toes and push off your foot as you walk. You rely on it virtually every time you walk and move your foot.
Rupture usually occurs in the section of the tendon situated within 2 1/2 inches (about 6 centimeters) of the point where it attaches to the heel bone. This section might be prone to rupture because blood flow is poor, which also can impair its ability to heal.
Ruptures often are caused by a sudden increase in the stress on your Achilles tendon. Common examples include:
- Increasing the intensity of sports participation, especially in sports that involve jumping
- Falling from a height
- Stepping into a hole
Risk factors
Factors that may increase your risk of Achilles tendon rupture include:
- Age. The peak age for Achilles tendon rupture is 30 to 40.
- Sex. Achilles tendon rupture is up to five times more likely to occur in men than in women.
- Recreational sports. Achilles tendon injuries occur more often during sports that involve running, jumping, and sudden starts and stops — such as soccer, basketball and tennis.
- Steroid injections. Doctors sometimes inject steroids into an ankle joint to reduce pain and inflammation. However, this medication can weaken nearby tendons and has been associated with Achilles tendon ruptures.
- Certain antibiotics. Fluoroquinolone antibiotics, such as ciprofloxacin (Cipro) or levofloxacin (Levaquin), increase the risk of Achilles tendon rupture.
- Obesity. Excess weight puts more strain on the tendon.
Prevention
 To reduce your chance of developing Achilles tendon problems, follow these tips:
To reduce your chance of developing Achilles tendon problems, follow these tips:
- Stretch and strengthen calf muscles. Stretch your calf until you feel a noticeable pull but not pain. Don't bounce during a stretch. Calf-strengthening exercises can also help the muscle and tendon absorb more force and prevent injury. To do the stretch, follow these steps:
- Stand at arm's length from a wall or a sturdy piece of exercise equipment. Put your palms flat against the wall or hold on to the piece of equipment.
- Keep one leg back with your knee straight and your heel flat on the floor.
- Slowly bend your elbows and front knee and move your hips forward until you feel a stretch in your calf.
- Hold this position for 30 to 60 seconds.
- Switch leg positions and repeat with your other leg.
- Vary your exercises. Alternate high-impact sports, such as running, with low-impact sports, such as walking, biking or swimming. Avoid activities that place excessive stress on your Achilles tendons, such as hill running and jumping activities.
- Choose running surfaces carefully. Avoid or limit running on hard or slippery surfaces. Dress properly for cold-weather training, and wear well-fitting athletic shoes with proper cushioning in the heels.
- Increase training intensity slowly. Achilles tendon injuries commonly occur after an abrupt increase in training intensity. Increase the distance, duration and frequency of your training by no more than 10 percent weekly.
Diagnosis & treatment
During the physical exam, your doctor will inspect your lower leg for tenderness and swelling. Your doctor might be able to feel a gap in your tendon if it has ruptured completely.
The doctor might ask you to kneel on a chair or lie on your stomach with your feet hanging over the end of the exam table. He or she might then squeeze your calf muscle to see if your foot will automatically flex. If it doesn't, you probably have ruptured your Achilles tendon.
If there's a question about the extent of your Achilles tendon injury — whether it's completely or only partially ruptured — your doctor might order an ultrasound or MRI scan. These painless procedures create images of the tissues of your body.
Treatment
Treatment for a ruptured Achilles tendon often depends on your age, activity level and the severity of your injury. In general, younger and more active people, particularly athletes, tend to choose surgery to repair a completely ruptured Achilles tendon, while older people are more likely to opt for nonsurgical treatment.
Recent studies, however, have shown fairly equal effectiveness of both surgical and nonsurgical management.
Nonsurgical treatment
This approach typically involves:
- Resting the tendon by using crutches
- Applying ice to the area
- Taking over-the-counter pain relievers
- Keeping the ankle from moving for the first few weeks, usually with a walking boot with heel wedges or a cast, with the foot flexed down
Nonoperative treatment avoids the risks associated with surgery, such as infection.
However, a nonsurgical approach might increase your chances of re-rupture and recovery can take longer, although recent studies indicate favorable outcomes in people treated nonsurgically if they start rehabilitation with weight bearing early.
Surgery
The procedure generally involves making an incision in the back of your lower leg and stitching the torn tendon together. Depending on the condition of the torn tissue, the repair might be reinforced with other tendons.
Complications can include infection and nerve damage. Minimally invasive procedures reduce infection rates over those of open procedures.
Rehabilitation
After either treatment, you'll have physical therapy exercises to strengthen your leg muscles and Achilles tendon. Most people return to their former level of activity within four to six months. It's important to continue strength and stability training after that because some problems can persist for up to a year.
A type of rehabilitation known as functional rehabilitation also focuses on coordination of body parts and how you move. The purpose is to return you to your highest level of performance, as an athlete or in your everyday life.
One review study concluded that if you have access to functional rehabilitation, you might do just as well with nonsurgical treatment as with surgery. More study is needed.
Rehabilitation after either surgical or nonsurgical management is also trending toward moving earlier and progressing faster. Studies are ongoing in this area also.
Preparing for your appointment
People with an Achilles tendon rupture commonly seek immediate treatment at a hospital's emergency department. You might also need to consult with doctors specializing in sports medicine or orthopedic surgery.
What you can do
Write a list that includes:
- Detailed descriptions of the symptoms and how and when the injury occurred
- Information about past medical problems
- All the medications and dietary supplements you take, including doses
- Questions to ask the doctor
What to expect from your doctor
The doctor may ask you some of the following questions:
- How did this injury occur?
- Did you feel or hear a popping or snapping sound when it happened?
- Can you stand on tiptoe on that foot?
Ankle arthritis: Psoriatic arthritis
 Psoriatic arthritis is a form of arthritis that affects some people who have psoriasis — a condition that features red patches of skin topped with silvery scales. Most people develop psoriasis first and are later diagnosed with psoriatic arthritis, but the joint problems can sometimes begin before skin patches appear.
Psoriatic arthritis is a form of arthritis that affects some people who have psoriasis — a condition that features red patches of skin topped with silvery scales. Most people develop psoriasis first and are later diagnosed with psoriatic arthritis, but the joint problems can sometimes begin before skin patches appear.
Joint pain, stiffness and swelling are the main signs and symptoms of psoriatic arthritis. They can affect any part of your body, including your fingertips and spine, and can range from relatively mild to severe. In both psoriasis and psoriatic arthritis, disease flares may alternate with periods of remission.
No cure for psoriatic arthritis exists, so the focus is on controlling symptoms and preventing damage to your joints. Without treatment, psoriatic arthritis may be disabling.
Symptoms
Both psoriatic arthritis and psoriasis are chronic diseases that get worse over time, but you may have periods when your symptoms improve or go into remission alternating with times when symptoms become worse.
Psoriatic arthritis can affect joints on just one side or on both sides of your body. The signs and symptoms of psoriatic arthritis often resemble those of rheumatoid arthritis. Both diseases cause joints to become painful, swollen and warm to the touch.
However, psoriatic arthritis is more likely to also cause:
- Swollen fingers and toes. Psoriatic arthritis can cause a painful, sausage-like swelling of your fingers and toes. You may also develop swelling and deformities in your hands and feet before having significant joint symptoms.
- Foot pain. Psoriatic arthritis can also cause pain at the points where tendons and ligaments attach to your bones — especially at the back of your heel (Achilles tendinitis) or in the sole of your foot (plantar fasciitis).
- Lower back pain. Some people develop a condition called spondylitis as a result of psoriatic arthritis. Spondylitis mainly causes inflammation of the joints between the vertebrae of your spine and in the joints between your spine and pelvis (sacroiliitis).
When to see a doctor
If you have psoriasis, be sure to tell your doctor if you develop joint pain. Psoriatic arthritis can severely damage your joints if left untreated.
Causes
Psoriatic arthritis occurs when your body's immune system begins to attack healthy cells and tissue. The abnormal immune response causes inflammation in your joints as well as overproduction of skin cells.
It's not entirely clear why the immune system attacks healthy tissue, but it seems likely that both genetic and environmental factors play a role. Many people with psoriatic arthritis have a family history of either psoriasis or psoriatic arthritis. Researchers have discovered certain genetic markers that appear to be associated with psoriatic arthritis.
Physical trauma or something in the environment — such as a viral or bacterial infection — may trigger psoriatic arthritis in people with an inherited tendency.
Risk factors
 Several factors can increase your risk of psoriatic arthritis, including:
Several factors can increase your risk of psoriatic arthritis, including:
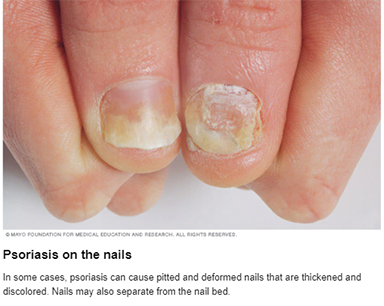
- Psoriasis. Having psoriasis is the single greatest risk factor for developing psoriatic arthritis. People who have pitted, deformed nails are especially likely to develop psoriatic arthritis.
- Your family history. Many people with psoriatic arthritis have a parent or a sibling with the disease.
- Your age. Although anyone can develop psoriatic arthritis, it occurs most often in adults between the ages of 30 and 50.
Complications
A small percentage of people with psoriatic arthritis develop arthritis mutilans — a severe, painful and disabling form of the disease. Over time, arthritis mutilans destroys the small bones in the hands, especially the fingers, leading to permanent deformity and disability.
People who have psoriatic arthritis sometimes also develop eye problems such as pinkeye (conjunctivitis) or uveitis, which can cause painful, reddened eyes and blurred vision. They are also at higher risk of cardiovascular disease.
Diagnosis & treatment
During the exam, your doctor may:
- Closely examine your joints for signs of swelling or tenderness
- Check your fingernails for pitting, flaking and other abnormalities
- Press on the soles of your feet and around your heels to find tender areas
No single test can confirm a diagnosis of psoriatic arthritis. But some types of tests can rule out other causes of joint pain, such as rheumatoid arthritis or gout.
Imaging tests
- X-rays. Plain X-rays can help pinpoint changes in the joints that occur in psoriatic arthritis but not in other arthritic conditions.
- Magnetic resonance imaging (MRI). MRI uses radio waves and a strong magnetic field to produce very detailed images of both hard and soft tissues in your body. This type of imaging test may be used to check for problems with the tendons and ligaments in your feet and lower back.
Laboratory tests
- Rheumatoid factor (RF). RF is an antibody that's often present in the blood of people with rheumatoid arthritis, but it's not usually in the blood of people with psoriatic arthritis. For that reason, this test can help your doctor distinguish between the two conditions.
- Joint fluid test. Using a needle, your doctor can remove a small sample of fluid from one of your affected joints — often the knee. Uric acid crystals in your joint fluid may indicate that you have gout rather than psoriatic arthritis.
Treatment
No cure exists for psoriatic arthritis, so treatment focuses on controlling inflammation in your affected joints to prevent joint pain and disability.
Medications
Drugs used to treat psoriatic arthritis include:
- NSAIDs. Nonsteroidal anti-inflammatory drugs (NSAIDs) can relieve pain and reduce inflammation. Over-the-counter NSAIDs include ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve). Stronger NSAIDs are available by prescription.
Side effects may include stomach irritation, heart problems, and liver and kidney damage. - Disease-modifying antirheumatic drugs (DMARDs). These drugs can slow the progression of psoriatic arthritis and save the joints and other tissues from permanent damage.
Common DMARDs include methotrexate (Trexall, Otrexup, others), leflunomide (Arava) and sulfasalazine (Azulfidine). Side effects vary but may include liver damage, bone marrow suppression and severe lung infections. - Immunosuppressants. These medications act to tame your immune system, which is out of control in psoriatic arthritis.
Examples include azathioprine (Imuran, Azasan) and cyclosporine (Gengraf, Neoral, Sandimmune). These medications can increase your susceptibility to infection. - Biologic agents. Also known as biologic response modifiers, this newer class of DMARDs includes abatacept (Orencia), adalimumab (Humira), certolizumab (Cimzia), etanercept (Enbrel), golimumab (Simponi), infliximab (Remicade), ixekizumab (Taltz), secukinumab (Cosentyx), tofacitinib (Xeljanz) and ustekinumab (Stelara).
These medications target specific parts of the immune system that trigger inflammation and lead to joint damage. These drugs can increase the risk of infections. Higher doses of tofacitinib can increase the risk of blood clots in the lungs. Biologic agents can be used alone or combined with DMARDs, such as methotrexate. - Newer oral medication. Apremilast (Otezla) decreases the activity of an enzyme in the body that controls the activity of inflammation within cells. Potential side effects include diarrhea, nausea and headaches.
Surgical and other procedures
- Steroid injections. This type of medication reduces inflammation quickly and is sometimes injected into an affected joint.
- Joint replacement surgery. Joints that have been severely damaged by psoriatic arthritis can be replaced with artificial prostheses made of metal and plastic.
Lifestyle and home remedies
- Protect your joints. Changing the way you carry out everyday tasks can make a tremendous difference in how you feel.
For example, you can avoid straining your finger joints by using gadgets such as jar openers to twist the lids from jars, by lifting heavy pans or other objects with both hands, and by pushing doors open with your whole body instead of just your fingers. - Maintain a healthy weight. Maintaining a healthy weight places less strain on your joints, leading to reduced pain and increased energy and mobility.
Losing weight if needed can also help your medications work better. Some psoriatic arthritis medications are less effective in people who have a body mass index of 25.0 to 29.9 (overweight).
The best way to increase nutrients while limiting calories is to eat more plant-based foods — fruits, vegetables and whole grains. - Exercise regularly. Exercise can help keep your joints flexible and your muscles strong. Types of exercises that are less stressful on joints include biking, swimming and walking.
- Stop smoking. Smoking is associated with a higher risk of developing psoriasis and with more-severe symptoms of psoriasis.
- Limit alcohol use. Alcohol can increase your risk of psoriasis, decrease the effectiveness of your treatment and increase side effects from some medications, such as methotrexate.
- Pace yourself. Battling pain and inflammation can leave you feeling exhausted. In addition, some arthritis medications can cause fatigue.
The key isn't to stop being active entirely, but to rest before you become too tired. Divide exercise or work activities into short segments. Find time to relax several times throughout the day.
Coping and support
Psoriatic arthritis can be particularly discouraging because the emotional pain that psoriasis can cause is compounded by joint pain and, in some cases, disability.
The support of friends and family can make a tremendous difference when you're facing the physical and psychological challenges of psoriatic arthritis. For some people, support groups can offer the same benefits.
A counselor or therapist can help you devise coping strategies to reduce your stress levels. The chemicals your body releases when you're under stress can aggravate both psoriasis and psoriatic arthritis.
Preparing for your appointment
You're likely to first discuss your signs and symptoms with your family doctor. He or she may refer you to a doctor specializing in the treatment of arthritis and related disorders (rheumatologist).
What you can do
Before your appointment, you may want to write a list of answers to the following questions:
- What types of symptoms are you having? When did they begin?
- Do you or any of your close family members have psoriasis?
- Has anyone in your immediate family ever had psoriatic arthritis?
- What medications and supplements do you take?
You may want to bring a friend or a family member with you to your appointment. It's hard to remember everything about a complicated condition, and another person may remember information that you miss.
What to expect from your doctor
Your doctor might ask some of the following questions:
- What joints are affected?
- Are there any activities or positions that make your symptoms better or worse?
- What treatments have you already tried? Have any of them helped?
Ankle arthritis: Reactive arthritis
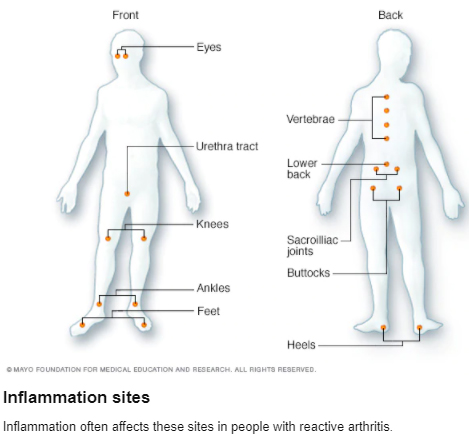
Reactive arthritis is joint pain and swelling triggered by an infection in another part of your body — most often your intestines, genitals or urinary tract.
Reactive arthritis usually targets your knees and the joints of your ankles and feet. Inflammation also can affect your eyes, skin and urethra.
Previously, reactive arthritis was sometimes called Reiter's syndrome, which was characterized by eye, urethra and joint inflammation.
Reactive arthritis isn't common. For most people, signs and symptoms come and go, eventually disappearing within 12 months.
Symptoms
 The signs and symptoms of reactive arthritis generally start one to four weeks after exposure to a triggering infection. They might include:
The signs and symptoms of reactive arthritis generally start one to four weeks after exposure to a triggering infection. They might include:
- Pain and stiffness. The joint pain associated with reactive arthritis most commonly occurs in your knees, ankles and feet. You also might have pain in your heels, low back or buttocks.
- Eye inflammation. Many people who have reactive arthritis also develop eye inflammation (conjunctivitis).
- Urinary problems. Increased frequency and discomfort during urination may occur, as can inflammation of the prostate gland or cervix.
- Inflammation of soft tissue where it enters bone (enthesitis). This might include muscles, tendons and ligaments.
- Swollen toes or fingers. In some cases, your toes or fingers might become so swollen that they resemble sausages.
- Skin problems. Reactive arthritis can affect your skin a variety of ways, including a rash on your soles and palms and mouth sores.
- Low back pain. The pain tends to be worse at night or in the morning.
When to see a doctor
If you develop joint pain within a month of having diarrhea or a genital infection, contact your doctor.
Causes
Reactive arthritis develops in reaction to an infection in your body, often in your intestines, genitals or urinary tract. You might not be aware of the triggering infection if it causes mild symptoms or none at all.
Numerous bacteria can cause reactive arthritis. Some are transmitted sexually, and others are foodborne. The most common ones include:
- Chlamydia
- Salmonella
- Shigella
- Yersinia
- Campylobacter
- Clostridium difficile
Reactive arthritis isn't contagious. However, the bacteria that cause it can be transmitted sexually or in contaminated food. Only a few of the people who are exposed to these bacteria develop reactive arthritis.
Risk factors
Certain factors increase your risk of reactive arthritis:
- Age. Reactive arthritis occurs most frequently in adults between the ages of 20 and 40.
- Sex. Women and men are equally likely to develop reactive arthritis in response to foodborne infections. However, men are more likely than are women to develop reactive arthritis in response to sexually transmitted bacteria.
- Hereditary factors. A specific genetic marker has been linked to reactive arthritis. But many people who have this marker never develop the condition.
Prevention
Genetic factors appear to play a role in whether you're likely to develop reactive arthritis. Though you can't change your genetic makeup, you can reduce your exposure to the bacteria that may lead to reactive arthritis.
Make sure your food is stored at proper temperatures and is cooked properly to help you avoid the many foodborne bacteria that can cause reactive arthritis, including salmonella, shigella, yersinia and campylobacter. Some sexually transmitted infections can trigger reactive arthritis. Using condoms might lower your risk.
Diagnosis & treatment
During the physical exam, your doctor is likely to check your joints for signs and symptoms of inflammation, such as swelling, warmth and tenderness, and test range of motion in your spine and affected joints. Your doctor might also check your eyes for inflammation and your skin for rashes.
Blood tests
Your doctor might recommend that a sample of your blood be tested for:
- Evidence of past or current infection
- Signs of inflammation
- Antibodies associated with other types of arthritis
- A genetic marker linked to reactive arthritis
Joint fluid tests
Your doctor might use a needle to withdraw a sample of fluid from within an affected joint. This fluid will be tested for:
- White blood cell count. An increased number of white blood cells might indicate inflammation or an infection.
- Infections. Bacteria in your joint fluid might indicate septic arthritis, which can result in severe joint damage.
- Crystals. Uric acid crystals in your joint fluid might indicate gout. This very painful type of arthritis often affects the big toe.
Imaging tests
X-rays of your low back, pelvis and joints can indicate whether you have any of the characteristic signs of reactive arthritis.
Treatment
The goal of treatment is to manage your symptoms and treat an infection that could still be present.
Medications
If your reactive arthritis was triggered by a bacterial infection, your doctor might prescribe an antibiotic if there is evidence of persistent infection. Which antibiotic you take depends on the bacteria that are present.
Other medications might include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs). Prescription NSAIDs, such as indomethacin (Indocin), can relieve the inflammation and pain of reactive arthritis.
- Corticosteroids. Injection of a corticosteroid into affected joints can reduce inflammation and allow you to return to your normal activity level.
- Topical steroids. These might be used for skin rashes caused by reactive arthritis.
- Rheumatoid arthritis drugs. Limited evidence suggests that medications such as sulfasalazine (Azulfidine), methotrexate (Trexall) or etanercept (Enbrel) can relieve pain and stiffness for some people with reactive arthritis.
Physical therapy
A physical therapist can provide you with targeted exercises for your joints and muscles. Strengthening exercises develop the muscles around your affected joints, which increase the joint's support. Range-of-motion exercises can increase your joints' flexibility and reduce stiffness.
Preparing for your appointment
You'll likely start by seeing your primary care provider, who might refer you to a doctor who specializes in arthritis (rheumatologist) for further evaluation.
What you can do
When you make the appointment, ask if there's anything you need to do in advance, such as fasting before having a specific test. Make a list of:
- Your symptoms, including any that seem unrelated to the reason for your appointment
- Key personal information, including your and your family's medical history
- All medications, vitamins or other supplements you take, including doses
- Questions to ask the doctor
Take a family member or friend along, if possible, to help you remember the information you're given. For reactive arthritis, basic questions to ask your doctor include:
- What is likely causing my symptoms or condition?
- What are other possible causes?
- What tests do I need? What treatment approach do you recommend?
- How soon do you expect my symptoms to improve with treatment?
- Is there anything I can do now to help relieve my joint pain?
- Am I at risk of long-term complications from this condition?
- I have these other health conditions. How can I best manage them together?
Don't hesitate to ask other questions.
What to expect from your doctor
Your doctor is likely to ask you a number of questions, such as:
- When did your symptoms begin?
- Have they been continuous or occasional?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
- Have you had a recent infection?
Ankle arthritis: Septic arthritis
Septic arthritis is a painful infection in a joint. The infection can come from germs that travel through your bloodstream from another part of your body. Septic arthritis can also occur when a penetrating injury delivers germs directly into the joint.
Infants and older adults are most likely to develop septic arthritis. Knees are most commonly affected, but septic arthritis also can affect hips, shoulders and other joints. The infection can quickly and severely damage the cartilage and bone within the joint, so prompt treatment is crucial.
Treatment involves draining the joint with a needle or surgically. Antibiotics also are usually needed to treat the infection.
Symptoms
Septic arthritis typically causes extreme discomfort and difficulty using the affected joint. The joint could be swollen, red and warm, and you might have a fever.
When to see a doctor
See your doctor if you have sudden onset of severe pain in a joint. Prompt treatment can help minimize joint damage.
Causes
Septic arthritis can be caused by bacterial, viral or fungal infections. Bacterial infection with Staphylococcus aureus (staph) is the most common cause. Staph commonly lives on even healthy skin.
Septic arthritis can develop when an infection, such as a skin infection or urinary tract infection, spreads through your bloodstream to a joint. Less commonly, a puncture wound, drug injection, or surgery in or near a joint can give the germs entry into the joint space.
The lining of your joints (synovium) has little ability to protect itself from infection. Your body's reaction to the infection — including inflammation that can increase pressure and reduce blood flow within the joint — contributes to the damage.
Risk factors
Risk factors for septic arthritis include:
- Existing joint problems. Chronic diseases and conditions that affect your joints — such as osteoarthritis, gout, rheumatoid arthritis or lupus — can increase your risk of septic arthritis, as can an artificial joint, previous joint surgery and joint injury.
- Taking medications for rheumatoid arthritis. People with rheumatoid arthritis have a further increase in risk because of medications they take that can suppress the immune system, making infections more likely to occur. Diagnosing septic arthritis in people with rheumatoid arthritis is difficult because many of the signs and symptoms are similar.
- Skin fragility. Skin that breaks easily and heals poorly can give bacteria access to your body. Skin conditions such as psoriasis and eczema increase your risk of septic arthritis, as do infected skin wounds. People who regularly inject drugs also have a higher risk of infection at the site of injection.
- Weak immune system. People with a weak immune system are at greater risk of septic arthritis. This includes people with diabetes, kidney and liver problems, and those taking drugs that suppress their immune systems.
- Joint trauma. Animal bites, puncture wounds or cuts over a joint can put you at risk of septic arthritis.
Having a combination of risk factors puts you at greater risk than having just one risk factor does.
Complications
If treatment is delayed, septic arthritis can lead to joint degeneration and permanent damage.
Diagnosis & treatment
The following tests typically help diagnose septic arthritis:
- Joint fluid analysis. Infections can alter the color, consistency, volume and makeup of the fluid within your joints. A sample of this fluid can be withdrawn from your affected joint with a needle. Laboratory tests can determine what organism is causing your infection, so your doctor will know which medications to prescribe.
- Blood tests. These can determine if there are signs of infection in your blood. A sample of your blood is removed from a vein with a needle.
- Imaging tests. X-rays and other imaging tests of the affected joint can assess damage to the joint.
Treatment
Doctors rely on joint drainage and antibiotic drugs to treat septic arthritis.
Joint drainage
Removing the infected joint fluid is crucial. Drainage methods include:
- Needle. In some cases, your doctor can withdraw the infected fluid with a needle inserted into the joint space.
- Scope procedure. In arthroscopy (ahr-THROS-kuh-pee), a flexible tube with a video camera at its tip is placed in your joint through a small incision. Suction and drainage tubes are then inserted through small incisions around your joint.
- Open surgery. Some joints, such as the hip, are more difficult to drain with a needle or arthroscopy, so an open surgical procedure might be necessary.
Antibiotics
To select the most effective medication, your doctor must identify the microbe causing your infection. Antibiotics are usually given through a vein in your arm at first. Later, you may be able to switch to oral antibiotics.
Typically, treatment lasts from two to six weeks. Antibiotics carry a risk of side effects, including nausea, vomiting and diarrhea. Allergic reactions also can occur. Ask your doctor about what side effects to expect from your medication.
Preparing for your appointment
If you have painful and inflamed joints, you're likely to start by seeing your family doctor. He or she may refer you to an orthopedic surgeon, infectious disease specialist or joint specialist (rheumatologist).
Here's some information to help you get ready for your appointment.
What you can do
When you call to make the appointment, ask if you need to do anything in advance, such as fasting for certain tests. Make a list of:
- Your symptoms, including any that may seem unrelated to the reason for which you scheduled the appointment
- Key personal information, including other medical conditions you have and recent infections
- Medications, vitamins or supplements you take, including doses
- Questions to ask your doctor
Take a family member or friend along, if possible, to help you remember information you're given.
For septic arthritis, questions to ask your doctor include:
- What is likely causing my symptoms?
- Are there other possible causes?
- What tests do I need?
- Is my condition likely temporary or chronic?
- What's the best course of action?
- Are there alternatives to the approach you're suggesting?
- How soon can I expect my symptoms to improve with treatment?
- What can I do in the meantime to help relieve my joint pain?
- Am I at risk of long-term complications from this condition?
- How can I best manage this condition with my other health problems?
- Should I see a specialist?
- Are there brochures or other printed material that I can take? What websites do you recommend?
Don't hesitate to ask other questions.
What to expect from your doctor
Your doctor is likely to ask you questions, such as:
- When did your symptoms begin?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
- Have you ever had joint surgery or joint replacement?
- Do you use recreational drugs?
Broken foot
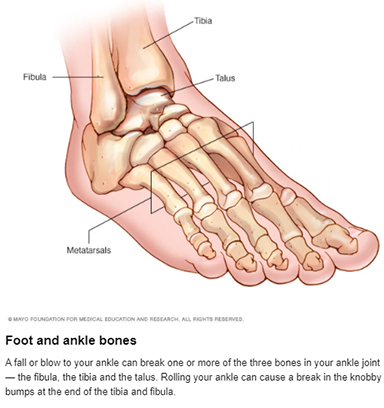 A broken foot is an injury to the bone. You may experience a broken foot during a car crash or from a simple misstep or fall.
A broken foot is an injury to the bone. You may experience a broken foot during a car crash or from a simple misstep or fall.
The seriousness of a broken foot varies. Fractures can range from tiny cracks in your bones to breaks that pierce your skin.
Treatment for a broken foot depends on the exact site and severity of the fracture. A severely broken foot may require surgery to implant plates, rods or screws into the broken bone to maintain proper position during healing.
Symptoms
If you have a broken foot, you may experience some of the following signs and symptoms:
- Immediate, throbbing pain
- Pain that increases with activity and decreases with rest
- Swelling
- Bruising
- Tenderness
- Deformity
- Difficulty in walking or bearing weight
When to see a doctor
See a doctor if there is obvious deformity, if the pain and swelling don't get better with self-care, or if the pain and swelling gets worse over time. Also, see a doctor if the injury interferes with walking.
Causes
The most common causes of a broken foot include:
- Car accidents. The crushing injuries common in car accidents may cause breaks that require surgical repair.
- Falls. Tripping and falling can break bones in your feet, as can landing on your feet after jumping down from just a slight height.
- Impact from a heavy weight. Dropping something heavy on your foot is a common cause of fractures.
- Missteps. Sometimes just putting your foot down wrong can result in a broken bone. A toe can get broken from stubbing your toes on furniture.
- Overuse. Stress fractures are common in the weight-bearing bones of your feet. These tiny cracks are usually caused over time by repetitive force or overuse, such as running long distances. But they can also occur with normal use of a bone that's been weakened by a condition such as osteoporosis.
Risk factors
You may be at higher risk of a broken foot or ankle if you:
- Participate in high-impact sports. The stresses, direct blows and twisting injuries that occur in sports such as basketball, football, gymnastics, tennis and soccer can causes foot fractures.
- Use improper technique or sports equipment. Faulty equipment, such as shoes that are too worn or not properly fitted, can contribute to stress fractures and falls. Improper training techniques, such as not warming up and stretching, also can cause foot injuries.
- Suddenly increase your activity level. Whether you're a trained athlete or someone who's just started exercising, suddenly boosting the frequency or duration of your exercise sessions can increase your risk of a stress fracture.
- Work in certain occupations. Certain work environments, such as a construction site, put you at risk of falling from a height or dropping something heavy on your foot.
- Keep your home cluttered or poorly lit. Walking around in a house with too much clutter or too little light may lead to falls and foot injuries.
- Have certain conditions. Having decreased bone density (osteoporosis) can put you at risk of injuries to your foot bones.
Complications
Complications of a broken foot are uncommon but may include:
- Arthritis. Fractures that extend into a joint can cause arthritis years later. If your foot starts to hurt long after a break, see your doctor for an evaluation.
- Bone infection (osteomyelitis). If you have an open fracture, meaning one end of the bone protrudes through the skin, your bone may be exposed to bacteria that cause infection.
- Nerve or blood vessel damage. Trauma to the foot can injure adjacent nerves and blood vessels, sometimes actually tearing them. Seek immediate attention if you notice any numbness or circulation problems. Lack of blood flow can cause a bone to die and collapse.
Prevention
These basic sports and safety tips may help prevent a broken foot:
- Wear proper shoes. Use hiking shoes on rough terrain. Wear steel-toed boots in your work environment if necessary. Choose appropriate athletic shoes for your sport.
- Replace athletic shoes regularly. Discard sneakers as soon as the tread or heel wears out or if the shoes are wearing unevenly. If you're a runner, replace your sneakers every 300 to 400 miles.
- Start slowly. That applies to a new fitness program and each individual workout.
- Cross-train. Alternating activities can prevent stress fractures. Rotate running with swimming or biking.
- Build bone strength. Calcium-rich foods, such as milk, yogurt and cheese, really can do your body good. Taking vitamin D supplements also can help.
- Use night lights. Many broken toes are the result of walking in the dark.
- Declutter your house. Keeping clutter off the floor can help you to avoid trips and falls.
Diagnosis & treatment
During the physical exam, your doctor will check for points of tenderness in your foot. The precise location of your pain can help determine its cause.
They may move your foot into different positions, to check your range of motion. You may be asked to walk for a short distance so that your doctor can examine your gait.
Imaging tests
If your signs and symptoms suggest a break or fracture, your doctor may suggest one or more of the following imaging tests.
- X-rays. Most foot fractures can be visualized on X-rays. The technician may need to take X-rays from several different angles so that the bone images won't overlap too much. Stress fractures often don't show up on X-rays until the break actually starts healing.
- Bone scan. For a bone scan, a technician will inject a small amount of radioactive material into a vein. The radioactive material is attracted to your bones, especially the parts of your bones that have been damaged. Damaged areas, including stress fractures, show up as bright spots on the resulting image.
- Computerized tomography (CT). CT scans take X-rays from many different angles and combine them to make cross-sectional images of internal structures of your body. CT scans can reveal more detail about the bone and the soft tissues that surround it, which may help your doctor determine the best treatment.
- Magnetic resonance imaging (MRI). MRI uses radio waves and a strong magnetic field to create very detailed images of the ligaments that help hold your foot and ankle together. This imaging helps to show ligaments and bones and can identify fractures not seen on X-rays.
Treatment
Treatments for a broken foot will vary, depending on which bone has been broken and the severity of the injury.
Medications
Your doctor may recommend an over-the-counter pain reliever, such as acetaminophen (Tylenol, others).
Therapy
After your bone has healed, you'll probably need to loosen up stiff muscles and ligaments in your feet. A physical therapist can teach you exercises to improve your flexibility and strength.
Surgical and other procedures
- Reduction. If you have a displaced fracture, meaning the two ends of the fracture are not aligned, your doctor may need to manipulate the pieces back into their proper positions — a process called reduction. Depending on the amount of pain and swelling you have, you may need a muscle relaxant, a sedative or even a general anesthetic before this procedure.
- Immobilization. To heal, a broken bone must be immobilized so that its ends can knit back together. In most cases, this requires a cast.
Minor foot fractures may only need a removable brace, boot or shoe with a stiff sole. A fractured toe is usually taped to a neighboring toe, with a piece of gauze between them. - Surgery. In some cases, an orthopedic surgeon may need to use pins, plates or screws to maintain proper position of your bones during healing. These materials may be removed after the fracture has healed if they are prominent or painful.
Preparing for your appointment
You will likely initially seek treatment for a broken foot in an emergency room or urgent care clinic. If the pieces of broken bone aren't lined up properly for healing, you may be referred to a doctor specializing in orthopedic surgery.
What you can do
You may want to write a list that includes:
- Detailed descriptions of your symptoms
- Information about medical problems you've had
- Information about the medical problems of your parents or siblings
- All the medications and dietary supplements you take
- Questions you want to ask the doctor
For a broken ankle or foot, basic questions to ask your doctor include:
- What tests are needed?
- What treatments are available, and which do you recommend?
- If I need a cast, how long will I need to wear it?
- Will I need surgery?
- What activity restrictions will need to be followed?
- Should I see a specialist?
- What pain medications do you recommend?
Don't hesitate to ask any other questions you have.
What to expect from your doctor
Your doctor may ask some of the following questions:
- Was there a specific injury that triggered your symptoms?
- Did your symptoms come on suddenly?
- Have you injured your feet in the past?
- Have you recently begun or intensified an exercise program?
What to do in the meantime
If your injury isn't severe enough to warrant a trip to the emergency room, here are some things you can do at home to care for your injury until you can see your doctor:
- Apply ice for 15 to 20 minutes at a time, every three to four hours to bring down the swelling.
- Keep your foot elevated.
- Don't put any weight on your injured foot.
- Lightly wrap the injury in a soft bandage that provides slight compression.
Bunions
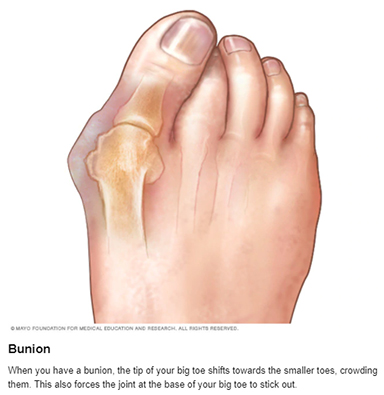 A bunion is a bony bump that forms on the joint at the base of your big toe. It occurs when some of the bones in the front part of your foot move out of place. This causes the tip of your big toe to get pulled toward the smaller toes and forces the joint at the base of your big toe to stick out. The skin over the bunion might be red and sore.
A bunion is a bony bump that forms on the joint at the base of your big toe. It occurs when some of the bones in the front part of your foot move out of place. This causes the tip of your big toe to get pulled toward the smaller toes and forces the joint at the base of your big toe to stick out. The skin over the bunion might be red and sore.
Wearing tight, narrow shoes might cause bunions or make them worse. Bunions can also develop as a result of the shape of your foot, a foot deformity or a medical condition, such as arthritis.
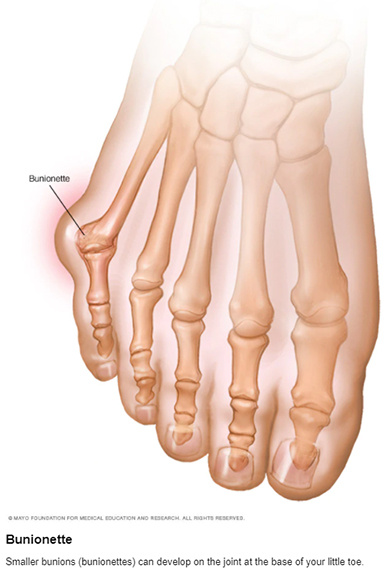
Smaller bunions (bunionettes) can develop on the joint of your little toe.
Symptoms
The signs and symptoms of a bunion include:
- A bulging bump on the outside of the base of your big toe
- Swelling, redness or soreness around your big toe joint
- Corns or calluses — these often develop where the first and second toes rub against each other
- Ongoing pain or pain that comes and goes
- Limited movement of your big toe
When to see a doctor
Although bunions often require no medical treatment, see your doctor or a doctor who specializes in treating foot disorders (podiatrist or orthopedic foot specialist) if you have:
- Ongoing big toe or foot pain
- A visible bump on your big toe joint
- Decreased movement of your big toe or foot
- Difficulty finding shoes that fit properly because of a bunion
Causes
There are many theories about how bunions develop, but the exact cause is unknown. Factors likely include:
- Inherited foot type
- Foot stress or injuries
- Deformities present at birth
Experts disagree on whether tight, high-heeled or too-narrow shoes cause bunions or whether footwear simply contributes to the development of bunions.
Bunions might be associated with certain types of arthritis, particularly inflammatory types, such as rheumatoid arthritis.
Risk factors
These factors might increase your risk of bunions:
- High heels. Wearing high heels forces your toes into the front of your shoes, often crowding your toes.
- Ill-fitting shoes. People who wear shoes that are too tight, too narrow or too pointed are more likely to develop bunions.
- Rheumatoid arthritis. Having this inflammatory condition can make you more likely to develop bunions.
- Heredity. The tendency to develop bunions might be the result of an inherited problem with the structure or anatomy of your foot.
Complications
Possible complications of bunions include:
- Bursitis. This painful condition occurs when the small fluid-filled pads that cushion the bones near your joints become inflamed.
- Hammertoe. An abnormal bend that occurs in the middle joint of a toe, usually the toe next to your big toe, can cause pain and pressure.
- Metatarsalgia. This condition causes pain and swelling in the ball of your foot.
Prevention
To help prevent bunions, choose shoes carefully. They should have a wide toe box — no pointy toes — and there should be space between the tip of your longest toe and the end of the shoe.
Your shoes should conform to the shape of your feet without squeezing or pressing any part of your foot.
Diagnosis & treatment
Your doctor can identify a bunion by examining your foot. After the physical exam, an X-ray of your foot can help your doctor determine the best way to treat it.
Treatment
Treatment options vary depending on the severity of your bunion and how much pain it causes.
Conservative treatment
Nonsurgical treatments that may relieve the pain and pressure of a bunion include:
- Changing shoes. Wear roomy, comfortable shoes that provide plenty of space for your toes.
- Padding. Over-the-counter, nonmedicated bunion pads or cushions may be helpful. They can act as a buffer between your foot and your shoe and ease your pain.
- Medications. Acetaminophen (Tylenol, others), ibuprofen (Advil, Motrin IB, others) or naproxen sodium (Aleve) can help you control the pain of a bunion. Cortisone injections also might help. .
- Shoe inserts. Padded shoe inserts can help distribute pressure evenly when you move your feet, reducing your symptoms and preventing your bunion from getting worse. Over-the-counter supports can provide relief for some people; others require prescription orthotic devices.
- Applying ice. Icing your bunion after you've been on your feet too long or if it becomes inflamed can help relieve soreness and swelling. If you have reduced feeling or circulation problems with your feet, check with your doctor first before applying ice.
Surgical options
If conservative treatment doesn't relieve your symptoms, you might need surgery. Surgery is not recommended for cosmetic reasons; only when a bunion causes you frequent pain or interferes with your daily activities.
There are many surgical procedures for bunions, and no one technique is best for every problem.
Surgical procedures for bunions can be done as single procedures or in combination. They might involve:
- Removing the swollen tissue from around your big toe joint
- Straightening your big toe by removing part of the bone
- Realigning one or more bones in the forefoot to a more normal position to correct the abnormal angle in your big toe joint
- Joining the bones of your affected joint permanently
It's possible that you'll be able to walk on your foot right after a bunion procedure. However, full recovery can take weeks to months.
To prevent a recurrence, you'll need to wear proper shoes after recovery. For most people, it's unrealistic to expect to wear narrower shoes after surgery.
Talk to your doctor about what you can expect after bunion surgery.
Preparing for your appointment
You're likely to start by seeing your primary care doctor or a foot specialist (podiatrist or orthopedic foot specialist).
What you can do
To make the most of your time with your doctor, prepare a list of questions before your visit. Your questions might include:
- What's causing my foot problems?
- Is this condition likely to be temporary or permanent?
- What treatment approach do you recommend?
- Am I a candidate for surgery? Why or why not?
- Are there other self-care steps that might help?
Don't hesitate to ask any other questions.
What to expect from your doctor
Some questions your doctor might ask include:
- When did you begin having foot problems?
- How much pain do you have in your foot?
- Where is the pain?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
- What type of shoes do you wear?
Flat feet
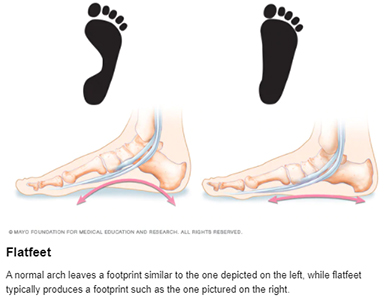 You have flatfeet when the arches on the inside of your feet are flattened, allowing the entire soles of your feet to touch the floor when you stand up.
You have flatfeet when the arches on the inside of your feet are flattened, allowing the entire soles of your feet to touch the floor when you stand up.
A common and usually painless condition, flatfeet can occur when the arches don't develop during childhood. In other cases, flatfeet develop after an injury or from the simple wear-and-tear stresses of age.
Flatfeet can sometimes contribute to problems in your ankles and knees because the condition can alter the alignment of your legs. If you aren't having pain, no treatment is usually necessary for flatfeet.
Diagnosis & treatment
To view the mechanics of your feet, your doctor will observe your feet from the front and back and ask you to stand on your toes. He or she might also look at the wear pattern on your shoes.
Imaging tests
If you're having a lot of pain in your feet, your doctor may order tests such as:
- X-rays. A simple X-ray uses a small amount of radiation to produce images of the bones and joints in your feet. It's particularly useful in detecting arthritis.
- CT scan. This test takes X-rays of your foot from different angles and provides much more detail than a standard X-ray.
- Ultrasound. If your doctor suspects an injured tendon, he or she may request this test, which uses sound waves to produce detailed images of soft tissues within the body.
- MRI. Using radio waves and a strong magnet, MRIs provide excellent detail of both hard and soft tissues.
Treatment
No treatment is necessary for flatfeet if they don't cause pain.
Therapy
If your flatfeet are painful, your doctor might suggest:
- Arch supports (orthotic devices). Over-the-counter arch supports may help relieve the pain caused by flatfeet. Or your doctor might suggest custom-designed arch supports, which are molded to the contours of your feet. Arch supports won't cure flatfeet, but they often reduce symptoms.
- Stretching exercises. Some people with flatfeet also have a shortened Achilles tendon. Exercises to stretch this tendon may help.
- Supportive shoes. A structurally supportive shoe might be more comfortable than sandals or shoes with minimal support.
- Physical therapy. Flatfeet may contribute to overuse injuries in some runners. A physical therapist can do a video analysis of how you run to help you improve your form and technique.
Surgery
Surgery isn't done solely to correct flatfeet. However, you might have surgery for an associated problem, such as a tendon tear or rupture.
Lifestyle and home remedies
If your flatfeet cause you minor pain, you might want to try:
- Rest. Avoid activities that aggravate your condition. Participate in low-impact activities — such as walking, biking or swimming — rather than jumping and running activities.
- Arch supports. Over-the-counter arch supports might increase your comfort.
- Medications. Over-the-counter pain relievers might help.
- Weight loss. Losing weight can reduce stress on your feet.
Preparing for your appointment
If your feet cause you significant pain, your family doctor may refer you to a doctor specializing in foot disorders (podiatrist) or sports medicine.
What you can do
Wear your everyday shoes to your appointment so your doctor can look at the wear patterns on the soles. Before the appointment, you might want to write answers to the following questions:
- When did you first notice problems with your feet?
- What other medical problems, if any, do you have?
- Do your parents or siblings have flatfeet?
- Have you ever injured your foot or ankle?
- What medications and supplements do you take regularly?
What to expect from your doctor
Your doctor may ask some of the following questions:
- Where exactly does it hurt?
- How would you describe the pain — dull, sharp, burning?
- Does any specific motion or position ease the pain or worsen it?
- Does the type of shoe you wear affect the pain?
- Can you stand on tiptoe on one foot?
- Have you tried arch supports?
- How does the pain affect your life?
Symptoms
Most people have no signs or symptoms associated with flatfeet. But some people with flatfeet experience foot pain, particularly in the heel or arch area. Pain may worsen with activity. Swelling along the inside of the ankle can also occur.
When to see a doctor
Talk to your doctor if you or your child has foot pain.
Causes
A flat foot is normal in infants and toddlers, because the foot's arch hasn't yet developed. Most people's arches develop throughout childhood, but some people never develop arches. This is a normal variation in foot type, and people without arches may or may not have problems.
Some children have flexible flatfoot, in which the arch is visible when the child is sitting or standing on tiptoes, but disappears when the child stands. Most children outgrow flexible flatfoot without problems.
Arches can also fall over time. Years of wear and tear can weaken the tendon that runs along the inside of your ankle and helps support your arch.
Risk factors
Factors that can increase your risk of flatfeet include:
- Obesity
- Injury to your foot or ankle
- Rheumatoid arthritis
- Aging
- Diabetes