
Recent Blogs
Dermatology Learn About Mohs Surgery
If you have a skin condition or your skin shows signs of aging, you may feel self-conscious. Feeling comfortable in your own skin is important. The dermatology experts understand that and are committed to helping restore your skin inside and out.
Dermatology experts provide a variety of cosmetic services and treatment for all types of skin diseases, from acne to rosacea. They also provide Mohs Surgery to treat skin cancer.
Learn more about common skin conditions treated by dermatology staff and skin rejuvenation treatments they provide. Call Dermatology with questions or to schedule a skin evaluation.
-
Acne
 Acne is a skin condition that occurs when your hair follicles become plugged with oil and dead skin cells. It often causes whiteheads, blackheads or pimples, and usually appears on the face, forehead, chest, upper back and shoulders. Acne is most common among teenagers, though it affects people of all ages.
Acne is a skin condition that occurs when your hair follicles become plugged with oil and dead skin cells. It often causes whiteheads, blackheads or pimples, and usually appears on the face, forehead, chest, upper back and shoulders. Acne is most common among teenagers, though it affects people of all ages.
Effective treatments are available, but acne can be persistent. The pimples and bumps heal slowly, and when one begins to go away, others seem to crop up.
Depending on its severity, acne can cause emotional distress and scar the skin. The earlier you start treatment, the lower your risk of such problems.
Symptoms
Acne signs and symptoms vary depending on the severity of your condition:
- Whiteheads (closed plugged pores)
- Blackheads (open plugged pores)
- Small red, tender bumps (papules)
- Pimples (pustules), which are papules with pus at their tips
- Large, solid, painful lumps beneath the surface of the skin (nodules)
- Painful, pus-filled lumps beneath the surface of the skin (cystic lesions)
When to see a doctor
If self-care remedies don't clear your acne, see your primary care doctor. He or she can prescribe stronger medications. If acne persists or is severe, you may want to seek medical treatment from a doctor who specializes in the skin (dermatologist).
For many women, acne can persist for decades, with flares common a week before menstruation. This type of acne tends to clear up without treatment in women who use contraceptives.
In older adults, a sudden onset of severe acne may signal an underlying disease requiring medical attention.
The Food and Drug Administration (FDA) warns that some popular nonprescription acne lotions, cleansers and other skin products can cause a serious reaction. This type of reaction is quite rare, so don't confuse it with the redness, irritation or itchiness where you've applied medications or products.
Seek emergency medical help if after using a skin product you experience:
- Faintness
- Difficulty breathing
- Swelling of the eyes, face, lips or tongue
- Tightness of the throat
-
Athlete's Foot
 Athlete's foot (tinea pedis) is a fungal infection that usually begins between the toes. It commonly occurs in people whose feet have become very sweaty while confined within tightfitting shoes.
Athlete's foot (tinea pedis) is a fungal infection that usually begins between the toes. It commonly occurs in people whose feet have become very sweaty while confined within tightfitting shoes.
Signs and symptoms of athlete's foot include a scaly rash that usually causes itching, stinging and burning. Athlete's foot is contagious and can be spread via contaminated floors, towels or clothing.
Athlete's foot is closely related to other fungal infections such as ringworm and jock itch. It can be treated with over-the-counter antifungal medications, but the infection often recurs. Prescription medications also are available.
Symptoms
Athlete's foot usually causes a scaly red rash. The rash typically begins in between the toes. Itching is often the worst right after you take off your shoes and socks.
Some types of athlete's foot feature blisters or ulcers. The moccasin variety of athlete's foot causes chronic dryness and scaling on the soles that extends up the side of the foot. It can be mistaken for eczema or even as dry skin.
The infection can affect one or both feet and can spread to your hand — especially if you scratch or pick at the infected parts of your feet.
When to see a doctor
If you have a rash on your foot that doesn't improve after self-treatment, see your doctor.
If you have diabetes, see your doctor if you suspect you have athlete's foot, especially if you notice any signs of a possible secondary bacterial infection such as excessive redness, swelling, drainage or fever.
Causes
Athlete's foot is caused by the same type of fungus that causes ringworm and jock itch. Damp socks and shoes and warm, humid conditions favor the organisms' growth.
Athlete's foot is contagious and can be spread by contact with an infected person or from contact with contaminated surfaces, such as towels, floors and shoes.
Risk factors
You are at higher risk of athlete's foot if you:
- Are a man
- Frequently wear damp socks or tightfitting shoes
- Share mats, rugs, bed linens, clothes or shoes with someone who has a fungal infection
- Walk barefoot in public areas where the infection can spread, such as locker rooms, saunas, swimming pools, communal baths and showers
Complications
Your athlete's foot infection can spread to other parts of your body, including:
- Your hand. People who scratch or pick at the infected parts of their feet may develop a similar infection in one of their hands.
- Your nails. The fungi associated with athlete's foot can also infect your toenails, a location that tends to be more resistant to treatment.
- Your groin. Jock itch is often caused by the same fungus that results in athlete's foot. It's common for the infection to spread from the feet to the groin as the fungus can travel on your hands or on a towel.
Prevention
These tips can help you avoid athlete's foot or ease the symptoms if infection occurs:
- Keep your feet dry, especially between your toes. Go barefoot to let your feet air out as much as possible when you're home. Dry between your toes after a bath or shower.
- Change socks regularly. If your feet get very sweaty, change your socks twice a day.
- Wear light, well-ventilated shoes. Avoid shoes made of synthetic material, such as vinyl or rubber.
- Alternate pairs of shoes. Don't wear the same pair every day so that you give your shoes time to dry after each use.
- Protect your feet in public places. Wear waterproof sandals or shoes around public pools, showers and lockers rooms.
- Treat your feet. Use powder, preferably antifungal, on your feet daily.
- Don't share shoes. Sharing risks spreading a fungal infection.
-
Cold Sore
 Cold sores — also called fever blisters — are a common viral infection. They are tiny, fluid-filled blisters on and around your lips. These blisters are often grouped together in patches. After the blisters break, a crust forms over the resulting sore.
Cold sores — also called fever blisters — are a common viral infection. They are tiny, fluid-filled blisters on and around your lips. These blisters are often grouped together in patches. After the blisters break, a crust forms over the resulting sore. Cold sores usually heal in two to four weeks without leaving a scar. Cold sores spread from person to person by close contact, such as kissing. They're caused by a herpes simplex virus (HSV-1) closely related to the one that causes genital herpes (HSV-2). Both of these viruses can affect your mouth or genitals and can be spread by oral sex. Cold sores are contagious even if you don't see the sores.
There's no cure for HSV infection, and the blisters may return. Antiviral medications can help cold sores heal more quickly and may reduce how often they return.
Symptoms
A cold sore usually passes through several stages:
- Tingling and itching. Many people feel an itching, burning or tingling sensation around their lips for a day or so before a small, hard, painful spot appears and blisters erupt.
- Blisters. Small fluid-filled blisters typically break out along the border where the outside edge of the lips meets the skin of the face. Cold sores can also occur around the nose or on the cheeks.
- Oozing and crusting. The small blisters may merge and then burst, leaving shallow open sores that will ooze fluid and then crust over.
Signs and symptoms vary, depending on whether this is your first outbreak or a recurrence. They can last several days, and the blisters can take two to four weeks to heal completely. Recurrences typically appear at the same spot each time and tend to be less severe than the first outbreak.
During first-time outbreaks, some people also experience:
- Fever
- Painful eroded gums
- Sore throat
- Headache
- Muscle aches
- Swollen lymph nodes
Children under 5 years old may have cold sores inside their mouths and the lesions are commonly mistaken for canker sores. Canker sores involve only the mucous membrane and aren't caused by the herpes simplex virus.
When to see a doctor
Cold sores generally clear up without treatment. See your doctor if:
- You have a weakened immune system
- The cold sores don't heal within two weeks
- Symptoms are severe
- You have frequent recurrences of cold sores
- You experience irritation in your eyes
Causes
Cold sores are caused by certain strains of the herpes simplex virus (HSV). HSV-1 usually causes cold sores. HSV-2 is usually responsible for genital herpes. However, either type can cause sores in the facial area or on the genitals. Most people who are infected with the virus that causes cold sores never develop signs and symptoms.
Cold sores are most contagious when oozing blisters are present. But you can transmit the virus to others even if you don't have blisters. Shared eating utensils, razors and towels, as well as kissing, may spread HSV-1. Oral sex can spread HSV-1 to the genitals and HSV-2 to the lips.
Once you've had an episode of herpes infection, the virus lies dormant in nerve cells in your skin and may emerge as another cold sore at the same place as before. Recurrence may be triggered by:
- Viral infection or fever
- Hormonal changes, such as those related to menstruation
- Stress
- Fatigue
- Exposure to sunlight and wind
- Changes in the immune system
Risk factors
About 90 percent of adults worldwide — even those who've never had symptoms of an infection — test positive for evidence of the virus that causes cold sores.
People who have weakened immune systems are at higher risk of complications from the virus. Medical conditions and treatments that increase your risk of complications include:
- HIV/AIDS
- Severe burns
- Eczema
- Cancer chemotherapy
- Anti-rejection drugs for organ transplants
Complications
In some people, the virus that causes cold sores can cause problems in other areas of the body, including:
- Fingertips. Both HSV-1 and HSV-2 can be spread to the fingers. This type of infection is often referred to as herpes whitlow. Children who suck their thumbs may transfer the infection from their mouths to their thumbs.
- Eyes. The virus can sometimes cause eye infection. Repeated infections can cause scarring and injury, which may lead to vision problems or blindness.
- Widespread areas of skin. People who have a skin condition called eczema are at higher risk of cold sores spreading all across their bodies. This can become a medical emergency.
- Other organs. In people with weakened immune systems, the virus can also affect organs such as the spinal cord and brain.
Prevention
Your doctor may prescribe an antiviral medication for you to take on a regular basis, if you develop cold sores frequently or if you're at high risk of serious complications. If sunlight seems to trigger your recurrences, apply sunblock to the spot where the cold sore tends to erupt.
To help avoid spreading cold sores to other people or to other parts of your body, you might try some of the following precautions:
- Avoid skin-to-skin contact with others while blisters are present. The virus spreads most easily when there are moist secretions from the blisters.
- Avoid sharing items. Utensils, towels, lip balm and other items can spread the virus when blisters are present.
- Keep your hands clean. When you have a cold sore, wash your hands carefully before touching yourself and other people, especially babies.
-
Common Warts
 Common warts are small, grainy skin growths that occur most often on your fingers or hands. Rough to the touch, common warts also often feature a pattern of tiny black dots — sometimes called seeds — which are small, clotted blood vessels.
Common warts are small, grainy skin growths that occur most often on your fingers or hands. Rough to the touch, common warts also often feature a pattern of tiny black dots — sometimes called seeds — which are small, clotted blood vessels.
Common warts are caused by a virus and are transmitted by touch. Children and young adults are more likely to develop common warts, as are people who have weakened immune systems. Common warts usually disappear on their own, but many people choose to remove them because they find them bothersome or embarrassing.
Symptoms
Common warts usually occur on your fingers or hands and may be:
- Small, fleshy, grainy bumps
- Flesh-colored, white, pink or tan
- Rough to the touch
- Sprinkled with black pinpoints, which are small, clotted blood vessels
When to see a doctor
See your doctor for common warts if:
- The growths are painful or change in appearance or color
- You've tried treating the warts, but they persist, spread or recur
- The growths are bothersome and interfere with activities
- You also have a weakened immune system because of immune-suppressing drugs, HIV/AIDS or other immune system disorders
- You aren't sure whether the growths are warts
Causes
Common warts are caused by an infection with the human papillomavirus (HPV). More than 100 types of HPV exist, but only a few cause warts on your hands. Other types of HPV are more likely to cause warts on your feet and other areas of your skin and mucous membranes. Most types of HPV cause relatively harmless conditions such as common warts, while others may cause serious disease such as cancer of the cervix.
You can get warts from skin-to-skin contact with people who have warts. If you have warts, you can spread the virus to other places on your own body. You can also get the wart virus indirectly by touching something that another person's wart touched, such as a towel or exercise equipment. The virus usually spreads through breaks in your skin, such as a hangnail or a scrape. Biting your nails also can cause warts to spread on your fingertips and around your nails.
Each person's immune system responds to the HPV virus differently, so not everyone who comes in contact with HPV develops warts.
Risk factors
People at higher risk of developing common warts include:
- Children and young adults
- People with weakened immune systems, such as those with HIV/AIDS or people who've had organ transplants
Prevention
To reduce your risk of common warts:
- Avoid direct contact with warts. This includes your own warts.
- Don't pick at warts. Picking may spread the virus.
- Don't use the same emery board, pumice stone or nail clipper on your warts as you use on your healthy skin and nails.
- Don't bite your fingernails. Warts occur more often in skin that has been broken. Nibbling the skin around your fingernails opens the door for the virus.
- Groom with care. Use a disposable emery board. And avoid brushing, clipping or shaving areas that have warts. If you must shave, use an electric razor.
- Wash your hands carefully after touching your warts or surfaces such as shared exercise equipment.
-
Atopic Dermatitis (Eczema)
 Atopic dermatitis (eczema) is a condition that makes your skin red and itchy. It's common in children but can occur at any age. Atopic dermatitis is long lasting (chronic) and tends to flare periodically. It may be accompanied by asthma or hay fever.
Atopic dermatitis (eczema) is a condition that makes your skin red and itchy. It's common in children but can occur at any age. Atopic dermatitis is long lasting (chronic) and tends to flare periodically. It may be accompanied by asthma or hay fever.
No cure has been found for atopic dermatitis. But treatments and self-care measures can relieve itching and prevent new outbreaks. For example, it helps to avoid harsh soaps, moisturize your skin regularly, and apply medicated creams or ointments.
Symptoms
Atopic dermatitis (eczema) signs and symptoms vary widely from person to person and include:
- Dry skin
- Itching, which may be severe, especially at night
- Red to brownish-gray patches, especially on the hands, feet, ankles, wrists, neck, upper chest, eyelids, inside the bend of the elbows and knees, and in infants, the face and scalp
- Small, raised bumps, which may leak fluid and crust over when scratched
- Thickened, cracked, scaly skin
- Raw, sensitive, swollen skin from scratching
Atopic dermatitis most often begins before age 5 and may persist into adolescence and adulthood. For some people, it flares periodically and then clears up for a time, even for several years.
When to see a doctor
See a doctor if you or your child:
- Is so uncomfortable that the condition is affecting sleep and daily activities
- Has a skin infection — look for red streaks, pus, yellow scabs
- Continues to experience symptoms despite trying home remedies
Seek immediate medical attention for your child if the rash looks infected and he or she has a fever.
Causes
Healthy skin helps retain moisture and protects you from bacteria, irritants and allergens. Eczema is related to a gene variation that affects the skin's ability to provide this protection. This allows your skin to be affected by environmental factors, irritants and allergens.
In some children, food allergies may play a role in causing eczema.
Risk factors
The primary risk factor for atopic dermatitis is having a personal or family history of eczema, allergies, hay fever or asthma.
Complications
Complications of atopic dermatitis (eczema) may include:
- Asthma and hay fever. Eczema sometimes precedes these conditions. More than half of young children with atopic dermatitis develop asthma and hay fever by age 13.
- Chronic itchy, scaly skin. A skin condition called neurodermatitis (lichen simplex chronicus) starts with a patch of itchy skin. You scratch the area, which makes it even itchier. Eventually, you may scratch simply out of habit. This condition can cause the affected skin to become discolored, thick and leathery.
- Skin infections. Repeated scratching that breaks the skin can cause open sores and cracks. These increase the risk of infection from bacteria and viruses, including the herpes simplex virus.
- Irritant hand dermatitis. This especially affects people whose work requires that their hands are often wet and exposed to harsh soaps, detergents and disinfectants.
- Allergic contact dermatitis. This condition is common in people with atopic dermatitis.
- Sleep problems. The itch-scratch cycle can cause poor sleep quality.
Prevention
The following tips may help prevent bouts of dermatitis (flares) and minimize the drying effects of bathing:
- Moisturize your skin at least twice a day. Creams, ointments and lotions seal in moisture. Choose a product or products that work well for you. Using petroleum jelly on your baby's skin may help prevent development of atopic dermatitis.
- Try to identify and avoid triggers that worsen the condition. Things that can worsen the skin reaction include sweat, stress, obesity, soaps, detergents, dust and pollen. Reduce your exposure to your triggers.
Infants and children may experience flares from eating certain foods, including eggs, milk, soy and wheat. Talk with your child's doctor about identifying potential food allergies. - Take shorter baths or showers. Limit your baths and showers to 10 to 15 minutes. And use warm, rather than hot, water.
- Take a bleach bath. The American Academy of Dermatology recommends considering a bleach bath to help prevent flares. A diluted-bleach bath decreases bacteria on the skin and related infections. Add 1/2 cup (118 milliliters) of household bleach, not concentrated bleach, to a 40-gallon (151-liter) bathtub filled with warm water. Measures are for a U.S.-standard-sized tub filled to the overflow drainage holes.
Soak from the neck down or just the affected areas of skin for about 10 minutes. Do not submerge the head. Take a bleach bath no more than twice a week. - Use only gentle soaps. Choose mild soaps. Deodorant soaps and antibacterial soaps can remove more natural oils and dry your skin.
- Dry yourself carefully. After bathing gently pat your skin dry with a soft towel and apply moisturizer while your skin is still damp.
-
Hair Loss
 Hair loss can affect just your scalp or your entire body. It can be the result of heredity, hormonal changes, medical conditions or medications. Anyone — men, women and children — can experience hair loss.
Hair loss can affect just your scalp or your entire body. It can be the result of heredity, hormonal changes, medical conditions or medications. Anyone — men, women and children — can experience hair loss.
Baldness typically refers to excessive hair loss from your scalp. Hereditary hair loss with age is the most common cause of baldness. Some people prefer to let their baldness run its course untreated and unhidden. Others may cover it up with hairstyles, makeup, hats or scarves. And still others choose one of the treatments available to prevent further hair loss and to restore growth.
Before pursuing hair loss treatment, talk with your doctor about the cause of the hair loss and the best treatment options.
Symptoms
Hair loss can appear in many different ways, depending on what's causing it. It can come on suddenly or gradually and affect just your scalp or your whole body. Some types of hair loss are temporary, and others are permanent.
Signs and symptoms of hair loss may include:
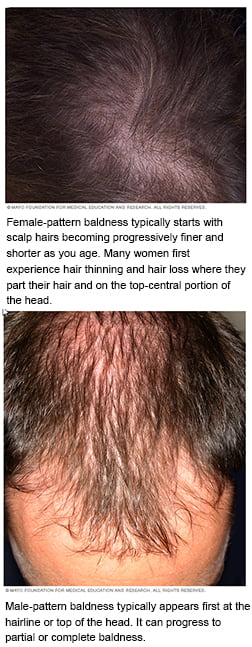
- Gradual thinning on top of head. This is the most common type of hair loss, affecting both men and women as they age. In men, hair often begins to recede from the forehead in a line that resembles the letter M. Women typically retain the hairline on the forehead but have a broadening of the part in their hair.
- Circular or patchy bald spots. Some people experience smooth, coin-sized bald spots. This type of hair loss usually affects just the scalp, but it sometimes also occurs in beards or eyebrows. In some cases, your skin may become itchy or painful before the hair falls out.
- Sudden loosening of hair. A physical or emotional shock can cause hair to loosen. Handfuls of hair may come out when combing or washing your hair or even after gentle tugging. This type of hair loss usually causes overall hair thinning and not bald patches.
- Full-body hair loss. Some conditions and medical treatments, such as chemotherapy for cancer, can result in the loss of hair all over your body. The hair usually grows back.
- Patches of scaling that spread over the scalp. This is a sign of ringworm. It may be accompanied by broken hair, redness, swelling and, at times, oozing.
When to see a doctor
See your doctor if your child or you are distressed by hair loss and want to pursue treatment. Also talk to your doctor if you notice sudden or patchy hair loss or more than usual hair loss when combing or washing your or your child's hair. Sudden hair loss can signal an underlying medical condition that requires treatment.
Causes
Most people normally shed 50 to 100 hairs a day. This usually doesn't cause noticeable thinning of scalp hair because new hair is growing in at the same time. Hair loss occurs when this cycle of hair growth and shedding is disrupted or when the hair follicle is destroyed and replaced with scar tissue.
The exact cause of hair loss may not be fully understood, but it's usually related to one or more of the following factors:
- Family history (heredity)
- Hormonal changes
- Medical conditions
- Medications
Family history (heredity)
The most common cause of hair loss is a hereditary condition called male-pattern baldness or female-pattern baldness. It usually occurs gradually and in predictable patterns — a receding hairline and bald spots in men and thinning hair in women.
Heredity also affects the age at which you begin to lose hair, the rate of hair loss and the extent of baldness. Pattern baldness is most common in men and can begin as early as puberty. This type of hair loss may involve both hair thinning and miniaturization (hair becomes soft, fine and short).
Hormonal changes and medical conditions
A variety of conditions can cause hair loss, including:
- Hormonal changes. Hormonal changes and imbalances can cause temporary hair loss. This could be due to pregnancy, childbirth or the onset of menopause. Hormone levels are also affected by the thyroid gland, so thyroid problems may cause hair loss.
- Patchy hair loss. This type of nonscarring hair loss is called alopecia areata (al-o-PEE-she-uh ar-e-A-tuh). It occurs when the body's immune system attacks hair follicles — causing sudden hair loss that leaves smooth, roundish bald patches on the skin.
- Scalp infections. Infections, such as ringworm, can invade the hair and skin of your scalp, leading to scaly patches and hair loss. Once infections are treated, hair generally grows back.
- Other skin disorders. Diseases that cause scarring alopecia may result in permanent loss at the scarred areas. These conditions include lichen planus, some types of lupus and sarcoidosis.
- Hair-pulling disorder. This condition, also called trichotillomania (trik-o-til-o-MAY-nee-uh), causes people to have an irresistible urge to pull out their hair, whether it's from the scalp, the eyebrows or other areas of the body.
Medications
Hair loss can be caused by drugs used for cancer, arthritis, depression, heart problems, high blood pressure and birth control. Intake of too much vitamin A may cause hair loss as well.
Other causes of hair loss
Hair loss can also result from:
- Radiation therapy to the head. The hair may not grow back the same as it was before.
- A trigger event. Many people experience a general thinning of hair several months after a physical or emotional shock. This type of hair loss is temporary. Examples of trigger events include sudden or excessive weight loss, a high fever, surgery, or a death in the family.
- Certain hairstyles and treatments. Excessive hairstyling or hairstyles that pull your hair tight, such as pigtails or cornrows, can cause traction alopecia. Hot oil hair treatments and permanents can cause inflammation of hair follicles that leads to hair loss. If scarring occurs, hair loss could be permanent.
Risk factors
A number of factors can increase your risk of hair loss, including:
- Family history
- Age
- Poor nutrition
- Certain medical conditions, such as diabetes and lupus
- Stress
Prevention
These tips may help you avoid preventable types of hair loss:
- Eat a nutritionally balanced diet.
- Avoid tight hairstyles, such as braids, buns or ponytails.
- Avoid compulsively twisting, rubbing or pulling your hair.
- Treat your hair gently when washing and brushing. A wide-toothed comb may help prevent pulling out hair.
- Avoid harsh treatments such as hot rollers, curling irons, hot oil treatments and permanents.
-
Chronic Hives
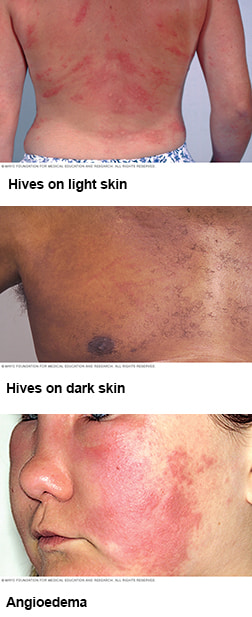 Hives (urticaria) are red, itchy welts that result from a skin reaction. The welts vary in size and appear and fade repeatedly as the reaction runs its course.
Hives (urticaria) are red, itchy welts that result from a skin reaction. The welts vary in size and appear and fade repeatedly as the reaction runs its course.
The condition is considered chronic hives if the welts appear for more than six weeks and recur frequently over months or years. Often, the cause of chronic hives is not clear.
Chronic hives can be very uncomfortable and interfere with sleep and daily activities. For many people, antihistamines and anti-itch medications provide relief.
Symptoms
Signs and symptoms of chronic hives include:
- Batches of red or skin-colored welts (wheals), which can appear anywhere on the body
- Welts that vary in size, change shape, and appear and fade repeatedly as the reaction runs its course
- Itching, which may be severe
- Painful swelling (angioedema) of the lips, eyelids and inside the throat
- A tendency for signs and symptoms to flare with triggers such as heat, exercise and stress
- A tendency for signs and symptoms to persist for more than six weeks and to recur frequently and unpredictably, sometimes for months or years
Short-term (acute) hives appear suddenly and clear up within a few weeks.
When to see a doctor
See your doctor if you have severe hives or hives that continue to appear for several days.
Seek emergency medical care
Chronic hives don't put you at any sudden risk of a serious allergic reaction (anaphylaxis). If you do experience hives as part of a serious allergic reaction, seek emergency care. Signs and symptoms of anaphylaxis include dizziness, trouble breathing, and swelling of your lips, eyelids and tongue.
Causes
The welts that come with hives arise when certain cells release histamine and other chemicals into your bloodstream.
Doctors often can't identify the reason for chronic hives or why acute hives sometimes turn into a long-term problem. The skin reaction may be triggered by:
- Pain medications
- Insects or parasites
- Infection
- Scratching
- Heat or cold
- Stress
- Sunlight
- Exercise
- Alcohol or food
- Pressure on the skin, as from a tight waistband
In some cases, chronic hives may be related to an underlying illness, such as a thyroid disease or, rarely, cancer.
Complications
Chronic hives don't put you at any sudden risk of a serious allergic reaction (anaphylaxis). But if you do experience hives as part of a serious allergic reaction, seek emergency care. Signs and symptoms of anaphylaxis include dizziness, trouble breathing, and swelling of your lips, eyelids and tongue.
-
Nail Problems
Problems with your fingernails or toenails could be a sign of a health problem. Consider seeing a dermatologist if your nails are thick, tough or painful or have scaling, white spots or red lines on them.

Ice pick-like depressions in the nails (nail pitting) are common in people who have psoriasis — a condition characterized by scaly patches on the skin. Nail pitting can also be related to connective tissue disorders, such as Reiter's syndrome, and alopecia areata — an autoimmune disease that causes hair loss.

Nail clubbing occurs when the tips of the fingers enlarge and the nails curve around the fingertips, usually over the course of years.
Nail clubbing is sometimes the result of low oxygen in the blood and could be a sign of various types of lung disease. Nail clubbing is also associated with inflammatory bowel disease, cardiovascular disease, liver disease and AIDS.
-
Psoriasis
 Psoriasis is a common skin condition that speeds up the life cycle of skin cells. It causes cells to build up rapidly on the surface of the skin. The extra skin cells form scales and red patches that are itchy and sometimes painful.
Psoriasis is a common skin condition that speeds up the life cycle of skin cells. It causes cells to build up rapidly on the surface of the skin. The extra skin cells form scales and red patches that are itchy and sometimes painful.
Psoriasis is a chronic disease that often comes and goes. The main goal of treatment is to stop the skin cells from growing so quickly.
There is no cure for psoriasis, but you can manage symptoms. Lifestyle measures, such as moisturizing, quitting smoking and managing stress, may help.
Symptoms
Psoriasis signs and symptoms are different for everyone. Common signs and symptoms include:
- Red patches of skin covered with thick, silvery scales
- Small scaling spots (commonly seen in children)
- Dry, cracked skin that may bleed
- Itching, burning or soreness
- Thickened, pitted or ridged nails
- Swollen and stiff joints
Psoriasis patches can range from a few spots of dandruff-like scaling to major eruptions that cover large areas.
Most types of psoriasis go through cycles, flaring for a few weeks or months, then subsiding for a time or even going into complete remission.
There are several types of psoriasis. These include:
- Plaque psoriasis. The most common form, plaque psoriasis causes dry, raised, red skin lesions (plaques) covered with silvery scales. The plaques might be itchy or painful and there may be few or many. They can occur anywhere on your body, including your genitals and the soft tissue inside your mouth.
- Nail psoriasis. Psoriasis can affect fingernails and toenails, causing pitting, abnormal nail growth and discoloration. Psoriatic nails might loosen and separate from the nail bed (onycholysis). Severe cases may cause the nail to crumble.
- Guttate psoriasis. This type primarily affects young adults and children. It's usually triggered by a bacterial infection such as strep throat. It's marked by small, water-drop-shaped, scaling lesions on your trunk, arms, legs and scalp.
The lesions are covered by a fine scale and aren't as thick as typical plaques are. You may have a single outbreak that goes away on its own, or you may have repeated episodes. - Inverse psoriasis. This mainly affects the skin in the armpits, in the groin, under the breasts and around the genitals. Inverse psoriasis causes smooth patches of red, inflamed skin that worsen with friction and sweating. Fungal infections may trigger this type of psoriasis.
- Pustular psoriasis. This uncommon form of psoriasis can occur in widespread patches (generalized pustular psoriasis) or in smaller areas on your hands, feet or fingertips.
It generally develops quickly, with pus-filled blisters appearing just hours after your skin becomes red and tender. The blisters may come and go frequently. Generalized pustular psoriasis can also cause fever, chills, severe itching and diarrhea. - Erythrodermic psoriasis. The least common type of psoriasis, erythrodermic psoriasis can cover your entire body with a red, peeling rash that can itch or burn intensely.
- Psoriatic arthritis. In addition to inflamed, scaly skin, psoriatic arthritis causes swollen, painful joints that are typical of arthritis. Sometimes the joint symptoms are the first or only manifestation of psoriasis or at times only nail changes are seen. Symptoms range from mild to severe, and psoriatic arthritis can affect any joint. Although the disease usually isn't as crippling as other forms of arthritis, it can cause stiffness and progressive joint damage that in the most serious cases may lead to permanent deformity.
When to see a doctor
If you suspect that you may have psoriasis, see your doctor for an examination. Also, talk to your doctor if your psoriasis:
- Causes you discomfort and pain
- Makes performing routine tasks difficult
- Causes you concern about the appearance of your skin
- Leads to joint problems, such as pain, swelling or inability to perform daily tasks
Seek medical advice if your signs and symptoms worsen or don't improve with treatment. You may need a different medication or a combination of treatments to manage the psoriasis.
Causes
The cause of psoriasis isn't fully understood, but it's thought to be related to an immune system problem with T cells and other white blood cells, called neutrophils, in your body.
T cells normally travel through the body to defend against foreign substances, such as viruses or bacteria.
But if you have psoriasis, the T cells attack healthy skin cells by mistake, as if to heal a wound or to fight an infection.
Overactive T cells also trigger increased production of healthy skin cells, more T cells and other white blood cells, especially neutrophils. These travel into the skin causing redness and sometimes pus in pustular lesions. Dilated blood vessels in psoriasis-affected areas create warmth and redness in the skin lesions.
The process becomes an ongoing cycle in which new skin cells move to the outermost layer of skin too quickly — in days rather than weeks. Skin cells build up in thick, scaly patches on the skin's surface, continuing until treatment stops the cycle.
Just what causes T cells to malfunction in people with psoriasis isn't entirely clear. Researchers believe both genetics and environmental factors play a role.
Psoriasis triggers
Psoriasis typically starts or worsens because of a trigger that you may be able to identify and avoid. Factors that may trigger psoriasis include:
- Infections, such as strep throat or skin infections
- Injury to the skin, such as a cut or scrape, a bug bite, or a severe sunburn
- Stress
- Smoking
- Heavy alcohol consumption
- Vitamin D deficiency
- Certain medications — including lithium, which is prescribed for bipolar disorder, high blood pressure medications such as beta blockers, antimalarial drugs, and iodides
Risk factors
Anyone can develop psoriasis, but these factors can increase your risk of developing the disease:
- Family history. This is one of the most significant risk factors. Having one parent with psoriasis increases your risk of getting the disease, and having two parents with psoriasis increases your risk even more.
- Viral and bacterial infections. People with HIV are more likely to develop psoriasis than people with healthy immune systems are. Children and young adults with recurring infections, particularly strep throat, also may be at increased risk.
- Stress. Because stress can impact your immune system, high stress levels may increase your risk of psoriasis.
- Obesity. Excess weight increases the risk of psoriasis. Lesions (plaques) associated with all types of psoriasis often develop in skin creases and folds.
- Smoking. Smoking tobacco not only increases your risk of psoriasis but also may increase the severity of the disease. Smoking may also play a role in the initial development of the disease.
Complications
If you have psoriasis, you're at greater risk of developing certain diseases. These include:
- Psoriatic arthritis. This complication of psoriasis can cause joint damage and a loss of function in some joints, which can be debilitating.
- Eye conditions. Certain eye disorders — such as conjunctivitis, blepharitis and uveitis — are more common in people with psoriasis.
- Obesity. People with psoriasis, especially those with more severe disease, are more likely to be obese. It's not clear how these diseases are linked, however. The inflammation linked to obesity may play a role in the development of psoriasis. Or it may be that people with psoriasis are more likely to gain weight, possibly because they're less active because of their psoriasis.
- Type 2 diabetes. The risk of type 2 diabetes rises in people with psoriasis. The more severe the psoriasis, the greater the likelihood of type 2 diabetes.
- High blood pressure. The odds of having high blood pressure are higher for people with psoriasis.
- Cardiovascular disease. For people with psoriasis, the risk of cardiovascular disease is twice as high as it is for those without the disease. Psoriasis and some treatments also increase the risk of irregular heartbeat, stroke, high cholesterol and atherosclerosis.
- Metabolic syndrome. This cluster of conditions — including high blood pressure, elevated insulin levels and abnormal cholesterol levels — increases your risk of heart disease.
- Other autoimmune diseases. Celiac disease, sclerosis and the inflammatory bowel disease called Crohn's disease are more likely to strike people with psoriasis.
- Parkinson's disease. This chronic neurological condition is more likely to occur in people with psoriasis.
- Kidney disease. Moderate to severe psoriasis has been linked to a higher risk of kidney disease.
- Emotional problems. Psoriasis can also affect your quality of life. Psoriasis is associated with low self-esteem and depression. You may also withdraw socially.
-
Rashes
Often called dermatitis, rashes can become itchy or painful. They have many causes, including allergic reactions, friction, prolonged exposure to heat and moisture, or contact with irritants, such as harsh chemicals. Hand eczema is a common rash. Many people with this problem start with dry, chapped hands that later become red, scaly and swollen.
Stasis dermatitis

Common signs and symptoms of stasis dermatitis include:
- Thickened, discolored (reddish) skin on the ankles or shins
- Itching
- Open sores, oozing and crusting
- Swelling
Stasis dermatitis occurs when varicose veins or other circulatory conditions cause fluids to build up in the lower legs. The swelling produces pressure beneath the skin and prevents adequate blood and oxygen from reaching the skin.
Allergic contact dermatitis

Common signs and symptoms of allergic contact dermatitis include:
- Red rash or bumps
- Blisters, draining fluid and crusting
- Itching and swelling
Allergic contact dermatitis results from direct contact with substances called allergens. It usually affects only the area that came into contact with the allergen. Common allergens include costume jewelry, perfume, cosmetics, hair dyes and poison ivy.
Atopic dermatitis

Common signs and symptoms of atopic dermatitis (eczema) include:
- Itching, which may be severe, and raw skin from scratching
- Small, raised bumps, which may leak fluid and crust over when scratched
- Red, leathery, cracked or scaly patches on the skin
Most often, atopic dermatitis occurs in the folds of the elbows, behind the knees and the front of the neck. It tends to flare periodically and then subside for a time, even up to several years. The exact cause of this skin disorder is unknown but is often seen in those with a personal or strong family history of asthma or allergic rhinitis (hay fever).
-
Rosacea
 Rosacea (roe-ZAY-she-uh) is a common skin condition that causes redness and visible blood vessels in your face. It may also produce small, red, pus-filled bumps. These signs and symptoms may flare up for a period of weeks to months and then diminish for a while. Rosacea can be mistaken for acne, an allergic reaction or other skin problems.
Rosacea (roe-ZAY-she-uh) is a common skin condition that causes redness and visible blood vessels in your face. It may also produce small, red, pus-filled bumps. These signs and symptoms may flare up for a period of weeks to months and then diminish for a while. Rosacea can be mistaken for acne, an allergic reaction or other skin problems.
Rosacea can occur in anyone. But it most commonly affects middle-aged women who have fair skin. While there's no cure for rosacea, treatments can control and reduce the signs and symptoms. If you experience persistent redness of your face, see your doctor for a diagnosis and proper treatment.
Symptoms
Signs and symptoms of rosacea may include:
- Facial redness. Rosacea usually causes a persistent redness in the central part of your face. Small blood vessels on your nose and cheeks often swell and become visible.
- Swollen red bumps. Many people who have rosacea also develop pimples on their face that resemble acne. These bumps sometimes contain pus. Your skin may feel hot and tender.
- Eye problems. About half of the people who have rosacea also experience eye dryness, irritation and swollen, reddened eyelids. In some people, rosacea's eye symptoms precede the skin symptoms.
- Enlarged nose. Rarely, rosacea can thicken the skin on the nose, causing the nose to appear bulbous (rhinophyma). This occurs more often in men than in women.
When to see a doctor
If you experience persistent redness of your face, see your doctor or a skin specialist (dermatologist) for a diagnosis and proper treatment.
Causes
The cause of rosacea is unknown, but it could be due to a combination of hereditary and environmental factors. Rosacea is not caused by poor hygiene.
A number of factors can trigger or aggravate rosacea by increasing blood flow to the surface of your skin. Some of these factors include:
- Hot drinks and spicy foods
- Alcohol
- Temperature extremes
- Sunlight or wind
- Emotions
- Exercise
- Cosmetics
- Drugs that dilate blood vessels, including some blood pressure medications
Risk factors
Anyone can develop rosacea. But you may be more likely to develop it if you:
- Are a woman
- Have fair skin, particularly if it has been damaged by the sun
- Are over age 30
- Smoke
- Have a family history of rosacea
Complications
In severe and rare cases, the oil glands (sebaceous glands) in your nose and sometimes your cheeks become enlarged, resulting in a buildup of tissue on and around your nose — a condition called rhinophyma (rie-no-FIE-muh). This complication is much more common in men and develops slowly over a period of years.
-
Skin Cancer
 Skin cancer — the abnormal growth of skin cells — most often develops on skin exposed to the sun. But this common form of cancer can also occur on areas of your skin not ordinarily exposed to sunlight.
Skin cancer — the abnormal growth of skin cells — most often develops on skin exposed to the sun. But this common form of cancer can also occur on areas of your skin not ordinarily exposed to sunlight.
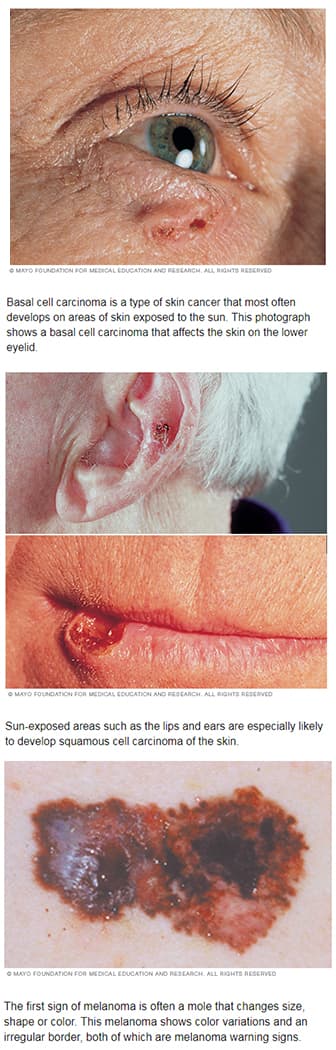
There are three major types of skin cancer — basal cell carcinoma, squamous cell carcinoma and melanoma.
You can reduce your risk of skin cancer by limiting or avoiding exposure to ultraviolet (UV) radiation. Checking your skin for suspicious changes can help detect skin cancer at its earliest stages. Early detection of skin cancer gives you the greatest chance for successful skin cancer treatment.
Symptoms
Where skin cancer develops
Skin cancer develops primarily on areas of sun-exposed skin, including the scalp, face, lips, ears, neck, chest, arms and hands, and on the legs in women. But it can also form on areas that rarely see the light of day — your palms, beneath your fingernails or toenails, and your genital area.
Skin cancer affects people of all skin tones, including those with darker complexions. When melanoma occurs in people with dark skin tones, it's more likely to occur in areas not normally exposed to the sun, such as the palms of the hands and soles of the feet.
Basal cell carcinoma signs and symptoms
Basal cell carcinoma usually occurs in sun-exposed areas of your body, such as your neck or face.
Basal cell carcinoma may appear as:
- A pearly or waxy bump
- A flat, flesh-colored or brown scar-like lesion
Squamous cell carcinoma signs and symptoms
Most often, squamous cell carcinoma occurs on sun-exposed areas of your body, such as your face, ears and hands. People with darker skin are more likely to develop squamous cell carcinoma on areas that aren't often exposed to the sun.
Squamous cell carcinoma may appear as:
- A firm, red nodule
- A flat lesion with a scaly, crusted surface
Melanoma signs and symptoms
Melanoma can develop anywhere on your body, in otherwise normal skin or in an existing mole that becomes cancerous. Melanoma most often appears on the face or the trunk of affected men. In women, this type of cancer most often develops on the lower legs. In both men and women, melanoma can occur on skin that hasn't been exposed to the sun.
Melanoma can affect people of any skin tone. In people with darker skin tones, melanoma tends to occur on the palms or soles, or under the fingernails or toenails.
Melanoma signs include:
- A large brownish spot with darker speckles
- A mole that changes in color, size or feel or that bleeds
- A small lesion with an irregular border and portions that appear red, white, blue or blue-black
- Dark lesions on your palms, soles, fingertips or toes, or on mucous membranes lining your mouth, nose, vagina or anus
Signs and symptoms of less common skin cancers
Other, less common types of skin cancer include:
- Kaposi sarcoma. This rare form of skin cancer develops in the skin's blood vessels and causes red or purple patches on the skin or mucous membranes.
Kaposi sarcoma mainly occurs in people with weakened immune systems, such as people with AIDS, and in people taking medications that suppress their natural immunity, such as people who've undergone organ transplants.
Other people with an increased risk of Kaposi sarcoma include young men living in Africa or older men of Italian or Eastern European Jewish heritage. - Merkel cell carcinoma. Merkel cell carcinoma causes firm, shiny nodules that occur on or just beneath the skin and in hair follicles. Merkel cell carcinoma is most often found on the head, neck and trunk.
- Sebaceous gland carcinoma. This uncommon and aggressive cancer originates in the oil glands in the skin. Sebaceous gland carcinomas — which usually appear as hard, painless nodules — can develop anywhere, but most occur on the eyelid, where they're frequently mistaken for other eyelid problems.
When to see a doctor
Make an appointment with your doctor if you notice any changes to your skin that worry you. Not all skin changes are caused by skin cancer. Your doctor will investigate your skin changes to determine a cause.
Causes
Skin cancer occurs when errors (mutations) occur in the DNA of skin cells. The mutations cause the cells to grow out of control and form a mass of cancer cells.
Cells involved in skin cancer
Skin cancer begins in your skin's top layer — the epidermis. The epidermis is a thin layer that provides a protective cover of skin cells that your body continually sheds. The epidermis contains three main types of cells:
- Squamous cells lie just below the outer surface and function as the skin's inner lining.
- Basal cells, which produce new skin cells, sit beneath the squamous cells.
- Melanocytes — which produce melanin, the pigment that gives skin its normal color — are located in the lower part of your epidermis. Melanocytes produce more melanin when you're in the sun to help protect the deeper layers of your skin.
Where your skin cancer begins determines its type and your treatment options.
Ultraviolet light and other potential causes
Much of the damage to DNA in skin cells results from ultraviolet (UV) radiation found in sunlight and in the lights used in tanning beds. But sun exposure doesn't explain skin cancers that develop on skin not ordinarily exposed to sunlight. This indicates that other factors may contribute to your risk of skin cancer, such as being exposed to toxic substances or having a condition that weakens your immune system.
Risk factors
Factors that may increase your risk of skin cancer include:
- Fair skin. Anyone, regardless of skin color, can get skin cancer. However, having less pigment (melanin) in your skin provides less protection from damaging UV radiation. If you have blond or red hair and light-colored eyes, and you freckle or sunburn easily, you're much more likely to develop skin cancer than is a person with darker skin.
- A history of sunburns. Having had one or more blistering sunburns as a child or teenager increases your risk of developing skin cancer as an adult. Sunburns in adulthood also are a risk factor.
- Excessive sun exposure. Anyone who spends considerable time in the sun may develop skin cancer, especially if the skin isn't protected by sunscreen or clothing. Tanning, including exposure to tanning lamps and beds, also puts you at risk. A tan is your skin's injury response to excessive UV radiation.
- Sunny or high-altitude climates. People who live in sunny, warm climates are exposed to more sunlight than are people who live in colder climates. Living at higher elevations, where the sunlight is strongest, also exposes you to more radiation.
- Moles. People who have many moles or abnormal moles called dysplastic nevi are at increased risk of skin cancer. These abnormal moles — which look irregular and are generally larger than normal moles — are more likely than others to become cancerous. If you have a history of abnormal moles, watch them regularly for changes.
- Precancerous skin lesions. Having skin lesions known as actinic keratoses can increase your risk of developing skin cancer. These precancerous skin growths typically appear as rough, scaly patches that range in color from brown to dark pink. They're most common on the face, head and hands of fair-skinned people whose skin has been sun damaged.
- A family history of skin cancer. If one of your parents or a sibling has had skin cancer, you may have an increased risk of the disease. A personal history of skin cancer. If you developed skin cancer once, you're at risk of developing it again.
- A weakened immune system. People with weakened immune systems have a greater risk of developing skin cancer. This includes people living with HIV/AIDS and those taking immunosuppressant drugs after an organ transplant.
- Exposure to radiation. People who received radiation treatment for skin conditions such as eczema and acne may have an increased risk of skin cancer, particularly basal cell carcinoma.
- Exposure to certain substances. Exposure to certain substances, such as arsenic, may increase your risk of skin cancer.
Prevention
Most skin cancers are preventable. To protect yourself, follow these skin cancer prevention tips:
-
Avoid the sun during the middle of the day. For many people in North America, the sun's rays are strongest between about 10 a.m. and 4 p.m. Schedule outdoor activities for other times of the day, even in winter or when the sky is cloudy.
You absorb UV radiation year-round, and clouds offer little protection from damaging rays. Avoiding the sun at its strongest helps you avoid the sunburns and suntans that cause skin damage and increase your risk of developing skin cancer. Sun exposure accumulated over time also may cause skin cancer. -
Wear sunscreen year-round. Sunscreens don't filter out all harmful UV radiation, especially the radiation that can lead to melanoma. But they play a major role in an overall sun protection program.
Use a broad-spectrum sunscreen with an SPF of at least 15. Apply sunscreen generously, and reapply every two hours — or more often if you're swimming or perspiring. Use a generous amount of sunscreen on all exposed skin, including your lips, the tips of your ears, and the backs of your hands and neck. - Wear protective clothing. Sunscreens don't provide complete protection from UV rays. So cover your skin with dark, tightly woven clothing that covers your arms and legs, and a broad-brimmed hat, which provides more protection than a baseball cap or visor does.
Some companies also sell photoprotective clothing. A dermatologist can recommend an appropriate brand.
Don't forget sunglasses. Look for those that block both types of UV radiation — UVA and UVB rays. - Avoid tanning beds. Lights used in tanning beds emit UV rays and can increase your risk of skin cancer.
- Be aware of sun-sensitizing medications. Some common prescription and over-the-counter drugs, including antibiotics, can make your skin more sensitive to sunlight.
Ask your doctor or pharmacist about the side effects of any medications you take. If they increase your sensitivity to sunlight, take extra precautions to stay out of the sun in order to protect your skin. -
Check your skin regularly and report changes to your doctor. Examine your skin often for new skin growths or changes in existing moles, freckles, bumps and birthmarks.
With the help of mirrors, check your face, neck, ears and scalp. Examine your chest and trunk, and the tops and undersides of your arms and hands. Examine both the front and back of your legs, and your feet, including the soles and the spaces between your toes. Also check your genital area and between your buttocks.
-
Skin Rejuvenation Treatments
Skin rejuvenation treatments and products are available to improve your skin’s overall appearance. We will carefully take care of your skin and find a solution that compliments you.
Treatments are safe, comfortable and effective without injections or surgery.
- Acne treatment: Chemical peel treatments work by exfoliating the skin’s surface to help inhibit the proliferation of acne bacteria and reducing oily complexions.
- Facial volume loss and deep wrinkles: Hyaluronic acid filler injections work by recreating facial volume that has been lost due to aging. Filler injections can help recreate the image of well-defined cheek bones, give volume to lips, and diminish the appearance of deep wrinkles around the mouth.
- Hydrating skin renewal: Procedure infuses serums, antioxidants and hyaluronic acid into the skin for softer, smoother and a more radiant, youthful complexion.
- Resurfacing: Chemical peels and/or laser treatments for resurfacing stimulates new collagen to grow, which improves your skin’s texture and tone to fight fine lines and wrinkles.
- Skin color: Treatments can diminish superficial pigmented and vascular marks. It will even your skin color and reduce tiny blood vessels.
- Wrinkles: Botulinum toxin injections help prevent and treat fine lines and wrinkles by preventing the muscles that cause those wrinkles from contracting.
Medical-grade skin products are available to help you keep your skin healthy and youthful.
Note: Please enter the building via Madison Avenue for your appointment.
Locations
Madison East Health Center
1400 Madison Ave., Suite 100AA, Mankato, MN 56001- Appointments:
- 507-594-2370
- Hours:
- Mon-Fri:8:00 AM - 5:00 PM
- Hours subject to change on holidays.
Enter the building via Madison Avenue for your appointment.





