
Pediatric & Adolescent Medicine (Children)
Recent Blogs
Children's Health and Parenting Resources
Whether you're a new parent or a seasoned veteran, you might have questions about infant and toddler health. The more you know about infant and toddler health, the more comfortable you'll feel caring for your child.
Start by sharing your questions with your child's doctor, then explore the health and safety topics below. Remember, nothing is too trivial when it comes to your child's health.
Breastfeeding
-
Breastfeeding and medications
Wondering about breastfeeding and medications? Know how medications can affect your breast milk and which drugs are safe to take.
If you're breastfeeding, you know you're giving your baby a healthy start. However, if you need to take medication while you're breastfeeding, you might have questions about the possible impact on your breast milk.
Here's what you need to know about medications and breastfeeding.
Do all medications pass into breast milk?
Almost any drug that's present in your blood will transfer into your breast milk to some extent. However, most medications do so at low levels and pose no real risk to most infants. There are exceptions, though, in which drugs can become concentrated in breast milk. As a result, every medication must be considered separately.
Does my baby's health and age influence how he or she might be affected by exposure to medication in my breast milk?
Yes. Exposure to medication in breast milk poses the greatest risk to premature babies, newborns, and babies who are medically unstable or have poorly functioning kidneys.
The risk is lowest for healthy babies 6 months and older, who can metabolize drugs efficiently. Women who breastfeed more than one year after childbirth often produce relatively smaller quantities of milk. This reduces the amount of medication transferred to breast milk. Also, medications used in the first three to four days after childbirth transfer at very low levels to an infant, due to the limited volume of breast milk you're producing.
Should I stop breastfeeding while taking medication?
Most medications are safe to take while breastfeeding. Also, the benefit of continuing to take a medication for a chronic condition while breastfeeding often outweighs any potential risks.
Still, a few medications aren't safe to take while breastfeeding. If you currently take a medication that could be harmful to your baby, your healthcare provider might be able to recommend a safe alternative medication. Or, he or she might recommend breastfeeding when the medication is at a low level in your breast milk.
In rare cases, your healthcare provider might recommend that you stop breastfeeding temporarily or permanently — depending on how long you need to take the medication. If you have advanced notice, pump in addition to breastfeeding and store surplus expressed milk for use during that time. If you need to stop breastfeeding only temporarily, use a double electric breast pump to keep up your milk supply until you're able to breastfeed again. Discard the milk you pump while you're taking the medication.
If you're not sure if a medication is compatible with breastfeeding, pump, clearly label and store expressed breast milk in a separate area until you can check with your healthcare provider.
If you need to stop breastfeeding permanently — which is unusual — ask your healthcare provider about weaning and to help you choose an infant formula that will meet your baby's needs.
What medications are safe to take while breastfeeding?
With your healthcare provider's input, consider this list of medications found to be safe during breastfeeding. Keep in mind that this isn't a comprehensive list of safe medications.
Pain relievers
- Acetaminophen (Tylenol, others)
- Ibuprofen (Advil, Motrin IB, others)
- Naproxen (Naprosyn®) — short-term use only
Antimicrobial medications
- Fluconazole (Diflucan)
- Miconazole (Monistat 3) — apply minimal amount
- Clotrimazole (Mycelex) — apply minimal amount
- Penicillins (amoxicillin, ampicillin, others)
- Cephalosporins (Keflex)
Antihistamines
- Loratadine (Claritin, Alavert, others)
- Fexofenadine (Allegra)
Decongestants
- Medications containing pseudoephedrine (Sudafed, Zyrtec D, others) — use with caution because pseudoephedrine can decrease milk supply
Birth control pills
- Progestin-only contraceptives, such as the minipill
New research suggests that combination birth control pills, oral contraceptives that contain estrogen and a progestin, don't affect milk production. However, further research is needed. To avoid possible interference with milk production, some experts recommend avoiding combination birth control methods during breastfeeding if possible. Otherwise, wait until breastfeeding is firmly established — about six to eight weeks — before using this type of birth control pill.
Keep in mind that combination birth control pills pose an increased risk of blood clots shortly after delivery. For otherwise healthy women, it's OK to begin using combined birth control pills and other types of combined hormonal birth control six weeks after childbirth.
Gastrointestinal medications
- Famotidine (Pepcid)
- Cimetidine (Tagamet HB)
Antidepressants
- Paroxetine (Paxil)
- Sertraline (Zoloft)
- Fluvoxamine (Luvox)
Constipation medications
- Docusate sodium (Colace)
Do I need my healthcare provider's OK ahead of time?
If you plan to take medication while breastfeeding, it's always best to check with your healthcare provider first. Avoid taking medications that aren't necessary, such as herbal medications, high-dose vitamins and unusual supplements.
Also ask about the timing. For example, taking medication immediately after breastfeeding might help minimize your baby's exposure. However, different drugs peak in breast milk at different times.
What if my baby has a reaction?
When you're taking medication, be sure to watch your baby for any unusual signs or symptoms — such as a change in eating or sleeping habits, fussiness, or a rash. If you notice any change in your baby's behavior, contact his or her doctor.
-
Breastfeeding nutrition
Breastfeeding nutrition can be confusing. How much should you eat? What should you avoid? How might your diet affect your baby? Follow these important nutrition tips.
If you're breastfeeding, you're giving your baby nutrients that will promote his or her growth and health. You might have questions, however, about what foods and drinks are best for you — and how your diet might affect your breast milk and your baby.
Understand the basics of breastfeeding nutrition.
Do I need extra calories while breastfeeding?
Yes, you might need to eat a little more — about an additional 400 to 500 calories a day — to keep up your energy.
To get these extra calories, opt for nutrient-rich choices, such as a slice of whole-grain bread with a tablespoon (about 16 grams) of peanut butter, a medium banana or apple, and 8 ounces (about 227 grams) of yogurt.
What foods should I eat while breastfeeding?
Focus on making healthy choices to help fuel your milk production. Opt for protein-rich foods, such as lean meat, eggs, dairy, beans, lentils and seafood low in mercury. Choose a variety of whole grains as well as fruits and vegetables. Wash your fruits and vegetables to reduce exposure to pesticide residue.
Eating a variety of different foods while breastfeeding will change the flavor of your breast milk. This will expose your baby to different tastes, which might help him or her more easily accept solid foods down the road.
To make sure you and your baby are getting all of the vitamins you need, your healthcare provider might recommend continuing to take a daily prenatal vitamin until you wean your baby.
How much fluid do I need while breastfeeding?
Drink frequently, preferably before you feel thirsty, and drink more if your urine appears dark yellow. Have a glass of water nearby when you breastfeed your baby.
Be wary of juices and sugary drinks, however. Too much sugar can contribute to weight gain — or sabotage your efforts to lose pregnancy weight. Too much caffeine can be troublesome, too. Limit yourself to no more than 2 to 3 cups (16 to 24 ounces) of caffeinated drinks a day. Caffeine in your breast milk might agitate your baby or interfere with your baby's sleep.
What about a vegetarian diet and breastfeeding?
If you follow a vegetarian diet, it's especially important to choose foods that'll give you the nutrients you need. For example:
- Choose foods rich in iron, protein and calcium. Good sources of iron include lentils, enriched cereals, whole-grain products, peas, dark leafy green vegetables and dried fruit. To help your body absorb iron, eat iron-rich foods with foods high in vitamin C, such as citrus fruits. For protein, consider eggs and dairy products or plant sources, such as soy products and meat substitutes, legumes, lentils, nuts, seeds, and whole grains. Good sources of calcium include dairy products and dark green vegetables. Other options include calcium-enriched and -fortified products, such as juices, cereals, soy milk, soy yogurt and tofu.
- Consider supplements. Your healthcare provider will likely recommend a daily vitamin B-12 supplement. Vitamin B-12 is found almost exclusively in animal products, so it's difficult to get enough in vegetarian diets. Vitamin B-12 is essential for your baby's brain development. If you don't eat enough vitamin D-fortified foods — such as cow's milk and some cereals — and you have limited sun exposure, you might need vitamin D supplements. Your baby needs vitamin D to absorb calcium and phosphorus. Too little vitamin D can cause rickets, a softening and weakening of bones. Tell your doctor and your baby's doctor if you're also giving your baby a vitamin D supplement.
What foods and drinks should I limit or avoid while breastfeeding?
Certain foods and drinks deserve caution while you're breastfeeding. For example:
- Alcohol. There's no level of alcohol in breast milk that's considered safe for a baby. If you drink, avoid breastfeeding until the alcohol has completely cleared your breast milk. This typically takes two to three hours for 12 ounces (355 milliliters) of 5 percent beer, 5 ounces (148 milliliters) of 11 percent wine or 1.5 ounces (44 milliliters) of 40 percent liquor, depending on your body weight. Pumping and dumping doesn't speed the elimination of alcohol from your body.
- Caffeine. Avoid drinking more than 2 to 3 cups (16 to 24 ounces) of caffeinated drinks a day. Caffeine in your breast milk might agitate your baby or interfere with your baby's sleep.
- Fish. Seafood can be a great source of protein and omega-3 fatty acids. Most seafood contains mercury or other contaminants, however. Exposure to excessive amounts of mercury through breast milk can pose a risk to a baby's developing nervous system. To limit your baby's exposure, avoid seafood that's high in mercury, including swordfish, king mackerel and tilefish. If you eat fish from local waters, pay attention to local fish advisories or limit fish from local waters to 6 ounces (170 grams) a week and don't eat other fish that week.
Could my diet cause my baby to be fussy or have an allergic reaction?
Certain foods or drinks in your diet could cause your baby to become irritable or have an allergic reaction. If your baby becomes fussy or develops a rash, diarrhea or congestion soon after nursing, consult your baby's doctor.
If you suspect that something in your diet might be affecting your baby, avoid the food or drink for up to a week to see if it makes a difference in your baby's behavior. Consider eliminating food made from cow's milk, peanuts, soy, wheat, eggs or corn. Some breastfeeding women say that avoiding spicy or gassy foods, such as onions or cabbage, can help — but this hasn't been proved through research.
To determine links between your diet and your baby's behavior, keep a food diary. List everything you eat and drink, along with notes about how your baby reacts — if at all. If removing a food or drink from your diet has no impact on your baby's fussiness, add it back to your diet and consider other culprits.
Remember, there's no need to go on a special diet while you're breastfeeding. Simply focus on making healthy choices — and you and your baby will reap the rewards.
-
Breastfeeding tips
Breastfeeding can be challenging. Consider breastfeeding tips for new moms, from asking for help right away to letting baby set the pace.
You know the benefits of breastfeeding. Breast milk contains the right balance of nutrients for your baby. Breast milk is easier to digest than is commercial formula, and the antibodies in breast milk boost your baby's immune system. Breastfeeding might even help you lose weight after the baby is born.
Still, breastfeeding can be challenging. Use these breastfeeding tips to get off to a good start.
Ask for help right away
Reading about breastfeeding is one thing. Doing it on your own is something else. The first time you breastfeed your baby — preferably within the first hour after delivery — ask for help.
The maternity nurses or a hospital lactation consultant can offer breastfeeding tips, starting with how to position the baby and make sure he or she is latching on correctly. Your doctor or your baby's doctor might offer breastfeeding tips, too.
Start by getting comfortable. Support yourself with pillows if needed. Then cradle your baby close to your breast — rather than learning forward to bring your breast to your baby. Support the baby's head with one hand and support your breast with the other hand. Tickle your baby's lower lip with your nipple to encourage your baby's mouth to open wide. He or she will take in part of the darker area around the nipple (areola). Your nipple will be far back in the baby's mouth, and the baby's tongue will be cupped under your breast. Look and listen for a rhythmic sucking and swallowing pattern.
If you need to remove the baby from your breast, first release the suction by inserting your finger into the corner of your baby's mouth.
Let your baby set the pace
For the first few weeks, most newborns breastfeed every two to three hours round-the-clock. Watch for early signs of hunger, such as stirring, restlessness, sucking motions and lip movements.
Let your baby nurse from the first breast thoroughly, until your breast feels soft — typically about 15 to 20 minutes. Keep in mind, however, that there is no set time. Then try burping the baby. After that, offer the second breast. If your baby's still hungry, he or she will latch on. If not, simply start the next breastfeeding session with the second breast. If your baby consistently nurses on only one breast at a feeding during the first few weeks, pump the other breast to relieve pressure and protect your milk supply.
Have your baby sleep in your room
Ideally, the baby should sleep in the same room as the parents for the first year of life — or at least for the first 6 months — to decrease the risk of SIDS. This can also make feeding easier.
Your baby should sleep alone in his or her own crib, bassinette or other surface designed for infants. Adult beds aren't safe for infants. A baby can become trapped and suffocate between the headboard slats, the space between the mattress and the bed frame, or the space between the mattress and the wall. A baby can also suffocate if a sleeping parent accidentally rolls over and covers the baby's nose and mouth.
Hold off on a pacifier
Some babies are happiest when they're sucking on something. Enter pacifiers — but there's a caveat. Giving your baby a pacifier too soon might interfere with breastfeeding, since sucking on a breast is different from sucking on a pacifier.
The American Academy of Pediatrics recommends waiting to introduce a pacifier until breastfeeding is well-established, usually three to four weeks after birth. Once you've settled into a breastfeeding routine, keep in mind that sucking on a pacifier at naptime or bedtime might reduce the risk of SIDS.
Gauge your success
When your baby is latched on successfully, you'll feel a gentle pulling sensation on your breast — rather than a pinching or biting sensation on your nipple. Your breasts might feel firm or full before the feeding, and softer or emptier afterward. Look for your baby to gain weight steadily, produce at least six wet diapers a day and be content between feedings. Your baby's stools will become yellow, seedy and loose.
Take care of your nipples
After each feeding, it's OK to let the milk dry naturally on your nipple. The milk can soothe your nipples. If you're in a hurry, gently pat your nipple dry. If your breasts leak between feedings, use bra pads — and change them often.
When you bathe, minimize the amount of soap, shampoo and other cleansers that might contact your nipples. If your nipples are dry or cracked, use purified lanolin (such as Lansinoh or Tender Care Lanolin) after each feeding. This can soothe cracked nipples, as well as help your nipples retain moisture.
Make healthy lifestyle choices
Your lifestyle choices are just as important when you're breastfeeding as they were when you were pregnant. For example:
- Eat a healthy diet. To keep up your energy, stick to healthy-eating basics, such as choosing plenty of fruits, vegetables and whole grains. Your healthcare provider might recommend taking a daily multivitamin as well.
- Drink plenty of fluids. Water, juice and milk can help you stay hydrated. Moderate amounts of caffeine are generally considered OK as well — but scale back if you suspect that too much caffeine is interfering with your baby's sleep. If you have an alcoholic drink, avoid breastfeeding for two hours afterward.
- Rest as much as possible. If you can, sleep when the baby sleeps.
- Don't smoke. Smoking during breastfeeding exposes babies to nicotine, which can interfere with your baby's sleep, as well as risks a cigarette burn to the baby. Secondhand smoke also increases the risk of sudden infant death syndrome (SIDS), as well as respiratory illnesses.
- Be cautious with medication. Many medications are safe to take while you're breastfeeding. Still, it's best to get your healthcare provider's OK first. If you have a chronic health condition, ask your healthcare provider if it's OK to breastfeed your baby.
Also ask your baby's doctor about vitamin D supplements for the baby, especially if you're exclusively breastfeeding. Breast milk might not provide enough vitamin D, which helps your baby absorb calcium and phosphorus — nutrients necessary for strong bones.
Give it time
If breastfeeding is tougher than you expected, try not to get discouraged. Feeding a newborn every few hours can be tiring, and it's OK to have a slow start. Just remember that the more often you breastfeed your baby, the more milk your breasts will produce — and the more natural breastfeeding is likely to feel.
Ask a lactation consultant or your baby's doctor for help if needed — especially if every feeding is painful or your baby isn't gaining weight. Although your nipples might be tender for the first few weeks, breastfeeding isn't supposed to hurt. If you haven't worked with a lactation consultant, ask your baby's doctor for a referral or check with the obstetrics department at a local hospital.
-
Breastfeeding twins
Planning to breastfeed more than one baby? Here's help breastfeeding twins or other multiples, from getting positioned and ensuring an adequate milk supply to combining breastfeeding and formula-feeding.
If you've decided to breastfeed your multiples, congratulations! Breastfeeding will provide many benefits for you and your babies. Still, breastfeeding more than one baby can be challenging. Understand how to get started and where to turn for support.
What are the benefits of breastfeeding twins or higher order multiples?
Breast milk contains the right balance of nutrients for your babies. The antibodies in breast milk will boost your babies' immune systems. Breast milk also has special benefits for babies who are born prematurely, as are many twins and higher order multiples. Breast milk is easier to digest than is commercial infant formula — especially for premature babies who have smaller, less mature stomachs and intestines. If your babies aren't able to nurse at first, you can pump breast milk to be given to your babies through a feeding tube.
Beyond the health benefits for your newborns, breastfeeding is likely the most convenient and least expensive way to feed your babies — and it might help you lose weight after you give birth. Breastfeeding twins or other multiples also ensures frequent interaction between you and each of your babies.
Should I breastfeed my babies at the same time?
When you start breastfeeding your babies, feed each one individually. This will give you a chance to see how well each baby latches on to your breast and address any issues. Consider creating a 24-hour chart to record how long and how often each baby nurses, as well as the number of wet and soiled diapers for each baby. If you feed your babies pumped breast milk, record how much they take at each feeding.
Once you've established breastfeeding with each baby, how you breastfeed is up to you and your babies. Some mothers find that breastfeeding two babies at once works well and saves time. Others prefer to breastfeed each baby separately. Likewise, some babies might show a preference for individual feedings. Try different approaches or a combination — such as breastfeeding one baby at a time at night and two at the same time during the day — to see what might work best.
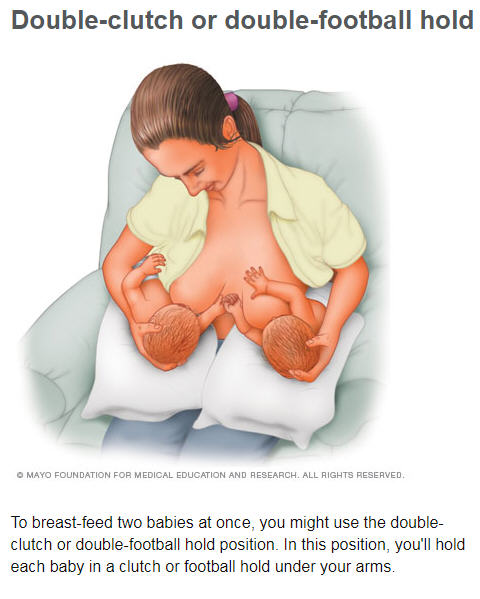
What positions can I use to breastfeed my babies at the same time?
There are several ways to breastfeed two babies at the same time. What's most important is choosing a position that feels good to you and your babies and enables a correct and comfortable latch.
For example:
- Double-clutch or double-football hold. In this position, you'll hold each baby in a clutch or football hold. Position a pillow on each side of your body and your lap. Place each baby on a pillow beside your body — almost under your arm — so that the babies' legs point toward the back of your chair. Make sure each baby's back is supported by the inside of your forearm. Use the pillows for arm support. Secure the babies' bottoms with the insides of your elbows. Keep the babies' heads at nipple level. Place the palm of one hand at the back of each baby's head to provide support. Alternatively, place both babies — head to head — on pillows directly in front of you. Be sure to keep your babies' bodies turned toward you, rather than facing up. Use your palms to support each baby's head.
- Cradle-clutch combination. In this position, you'll hold one baby in the cradle position — with his or her head on your forearm and his or her whole body facing yours — and the other baby in the clutch position. If one of your babies has an easier time latching on to your breast or staying latched, place him or her in the cradle position.
- Double-cradle hold. To use the double-cradle position, you'll place both of your babies in the cradle position in front of you. Position your babies so that their legs overlap and make an X across your lap.
At first, you might want help positioning your babies. Enlist someone to help you get situated until you get the hang of simultaneous feedings. Consider latching first the baby who tends to need more help getting started.
Will I have enough milk?
Most women are able to produce enough milk to feed twins. Many women are also able to breastfeed or pump enough breast milk to feed higher order multiples. To ensure a steady milk supply, consider these tips:
- Start right after birth. Breastfeeding your newborns soon after birth and at least eight to 12 times every 24 hours will help you establish your milk supply. The more often you breastfeed, the more milk you'll produce.
- Pump. If your babies are born early and are unable to breastfeed right away, begin pumping shortly after you give birth to establish your milk supply. Hospital-grade, double electric breast pumps help stimulate milk production while cutting pumping time in half. Once breastfeeding is well-established, pumping also allows other caregivers to help with feedings.
- Alternate breasts. Offering both breasts to each baby at each feeding and alternating the breast the feedings are started on, as well as which baby feeds first, might optimize your milk production and each baby’s feeding. This is because each of your babies might have a different style of feeding. Switching breasts will also give your babies different views, which stimulates their eyes. Consider assigning each baby to one breast for a day and then switching the next day or giving each baby a different breast at each feeding.
Remember to always bring your babies to your breast — rather than bending over or leaning forward to bring your breast to your babies.
Can I combine breastfeeding and formula-feeding?
Exclusive breastfeeding is recommended. Once breastfeeding is established and if you have chosen to do an occasional bottle, expressed breast milk would be the best choice so that formula could be avoided or delayed.
However, some mothers choose to combine breastfeeding and formula-feeding. For example, you might replace one or more breastfeeding sessions with a formula-feeding. Work with your doctor, your baby's doctor and a lactation consultant to determine what works best for you and your babies. If you give your babies formula, keep in mind that your milk production might begin to decrease if you breast-feed or pump less than eight to 10 times within 24 hours.
What else do I need to know about breastfeeding twins or higher order multiples?
Getting the hang of breastfeeding twins or other multiples can be difficult, but don't get discouraged. If you're struggling, meet with a lactation consultant who has experience with multiples. Ask your baby's doctor for help. Talk to other women who successfully breastfed multiples. Ask loved ones for assistance with household tasks and the care of older siblings — or consider hiring household help — so that you can focus on feeding and caring for your babies.
Be patient with yourself and your babies as you experience the challenges and rewards of breastfeeding two or more newborns. Above all, don't be afraid to ask for help.
-
Breastfeeding vs. formula-feeding
The benefits of breastfeeding are well established. Consider ways to support breastfeeding — and how to handle feelings of guilt if you can't or decide not to breastfeed.
Breastfeeding is the recommended way to feed a newborn. Depending on the circumstances, however, various factors might lead you to consider formula-feeding.
How long should I breastfeed my baby?
The American Academy of Pediatrics recommends exclusive breastfeeding for the first six months after birth and breastfeeding in combination with solid foods until at least age 1. Extended breastfeeding is recommended as long as you and your baby wish to continue.
Breast milk contains the right balance of nutrients for your baby and boosts your baby's immune system. It's considered the gold standard for infant nutrition.
Is any additional nutrition necessary?
Ask your baby's doctor about vitamin D supplements for the baby, especially if you're exclusively breastfeeding. Breast milk might not provide enough vitamin D, which helps your baby absorb calcium and phosphorus — nutrients necessary for strong bones.
What can I do to promote successful breastfeeding?
Taking care of yourself can go a long way toward promoting successful breastfeeding. Eat a healthy diet, drink plenty of fluids and rest as much as possible.
To boost your confidence, learn as much as you can about breastfeeding. Keep the environment calm and relaxed. Look to your partner and other loved ones for support. Don't be afraid to ask for help. Friends who've successfully breast-fed might be a good source of information. Lactation consultants are available at many hospitals and clinics. Your baby's doctor might be able to help, too.
What if breastfeeding isn't going well?
If you're struggling, ask a lactation consultant or your baby's doctor for help. If your baby's doctor is concerned that your baby isn't receiving adequate nutrition or hydration, he or she might suggest pumping and supplementing with expressed breast milk or formula.
Breast milk is the ideal food for babies — and the best way to keep a baby healthy — but proper nutrition and hydration are absolutely essential for your baby.
Does infant formula pose any risks to a baby?
Commercial infant formulas don't contain the immunity-boosting elements of breast milk. For most babies, breast milk is also easier to digest than formula. When prepared as directed, however, infant formula supports healthy babies who have typical dietary needs. A baby who has special nutritional needs might require a special formula.
Can I combine breastfeeding and formula-feeding?
Exclusive breastfeeding is recommended for the first six months after birth. A diet of breast milk only provides the best nutrition. Formula supplementation can disrupt breastfeeding as well as affect milk supply. However, some mothers are able to combine breastfeeding and formula-feeding — especially after breastfeeding has been well-established.
If I choose not to breastfeed, how should I handle the resulting emotions?
If you're considering formula-feeding, do your research so that you can make an informed decision. Then focus on nourishing and nurturing your baby — instead of dwelling on negative emotions. You might also share your feelings with your doctor, your baby's doctor or others in your support circle.
Remember, parenting is an adventure that requires choices and compromises. What counts is doing the best you can as you face this new challenge.
-
Breast Milk Storage
Breast milk storage can be confusing. Follow these practical tips on choosing containers, freezing breast milk, thawing breast milk and more.
If you're breastfeeding and going back to work or looking for more flexibility, you're probably considering using a breast pump. Once you start pumping, it's important to know how to safely store your expressed milk. Consider these do's and don'ts for breast milk storage.
What kind of container should I use to store expressed breast milk?
Before expressing or handling breast milk, wash your hands with soap and water. Then store the expressed milk in a clean, capped glass or hard plastic, BPA-free container. You can also use special plastic bags designed for milk collection and storage.
However, breast milk storage bags might tear, leak and become contaminated more easily than hard-sided containers. For extra protection, place the bags in a hard plastic food storage container with a tightly sealed lid.
Don't store breast milk in disposable bottle liners or plastic bags designed for general household use.
What's the best way to store expressed breast milk?
Using waterproof labels and ink, label each container with the date you expressed the breast milk. If you're storing expressed milk at your baby's child care facility, add your baby's name to the label. Place the containers in the back of the refrigerator or freezer, where the temperature is the coolest. If you don't have access to a refrigerator or freezer, store the milk temporarily in an insulated cooler.
Fill individual containers with the milk your baby will need for one feeding. You might start with 2 to 4 ounces (59 to 118 milliliters), and then adjust as needed. Also consider storing smaller portions — 1 to 2 ounces (30 to 59 milliliters) — for unexpected situations or delays in regular feedings. Breast milk expands as it freezes, so don't fill containers to the brim.
Can I add freshly expressed breast milk to already stored milk?
You can add freshly expressed breast milk to refrigerated or frozen milk you expressed earlier in the same day. However, thoroughly cool the freshly expressed breast milk in the refrigerator or a cooler with ice packs before adding it to previously chilled or frozen milk. Don't add warm breast milk to frozen breast milk because it will cause the frozen milk to partially thaw.
How long does expressed breast milk keep?
How long you can safely keep expressed breast milk depends on the storage method. Consider these general guidelines for healthy infants:
- Room temperature. Freshly expressed breast milk can be kept at room temperature for up to six hours. However, use or proper storage within four hours is optimal. If the room is especially warm, the limit is also four hours.
- Insulated cooler. Freshly expressed breast milk can be stored in an insulated cooler with ice packs for up to one day.
- Refrigerator. Freshly expressed breast milk can be stored in the back of the refrigerator for up to five days in clean conditions. However, use or freezer storage within three days is optimal.
- Deep freezer. Freshly expressed breast milk can be stored in the back of a deep freezer for up to 12 months. However, using the frozen milk within six months is optimal.
Keep in mind research suggests that the longer you store breast milk — whether in the refrigerator or in the freezer — the greater the loss of vitamin C in the milk. It's also important to note that breast milk expressed when a baby is a newborn won't as completely meet the same baby's needs when he or she is a few months older. Also, storage guidelines might differ for preterm, sick or hospitalized infants.
How do I thaw frozen breast milk?
Thaw the oldest milk first. Place the frozen container in the refrigerator the night before you intend to use it. You can also gently warm the milk by placing it under warm running water or in a bowl of warm water.
Also, don't heat a frozen bottle in the microwave or very quickly on the stove. Some parts of the milk might be too hot, and others cold. Some research suggests that rapid heating can affect the milk's antibodies.
While further research is needed on whether previously frozen milk that's been thawed can be frozen again and safely used, many experts recommend discarding thawed milk that isn't used within 24 hours.
Does thawed breast milk smell or look different from fresh breast milk?
The color of your breast milk might vary, depending on your diet. Also, thawed breast milk might seem to have a different odor or consistency than freshly expressed milk. It's still safe to feed to your baby. If your baby refuses the thawed milk, it might help to shorten the storage time.
-
Breastfeeding: How to gauge success
If you're breastfeeding, you might wonder whether your baby is getting enough milk. Ask yourself these questions — and know when to seek help.
When you're breastfeeding, you might not always know the exact amount of milk your baby drinks during each feeding — but you can still make sure your baby is getting enough to eat.
Here's how.
Cover the basics
When you're breastfeeding, ask yourself these questions:
- Is your baby gaining weight? Steady weight gain is often the most reliable sign that a baby is getting enough to eat. Although most babies lose weight soon after birth, it's typically regained within one to two weeks. Your baby will be weighed at each checkup. If you're concerned about your baby's weight, make an appointment to have your baby weighed.
- How often does your baby breastfeed? Most newborns breastfeed eight to 12 times a day — about every two to three hours. During growth spurts, your baby might take more at each feeding or want to breastfeed more often. Trust your body's ability to keep up with the increased demand. The more often your baby nurses, the more milk your breasts produce. As your baby gets older, he or she will take in more milk in less time at each feeding.
- Is your baby swallowing? If you look and listen carefully, you'll be able to tell when your baby is swallowing — usually after several sucks in a row. You'll hear a soft "k" sound and see a ripple under your baby's chin and lower jaw. If your baby swallows quietly, you might only notice a pause in his or her breathing.
- How do your breasts feel? When your baby is latched on successfully, you'll feel a gentle pulling sensation on your breast — rather than a pinching or biting sensation on your nipple. Your breasts might feel firm or full before the feeding, and softer or emptier afterward. If breastfeeding hurts, ask your baby's doctor or a lactation consultant for help.
- What about your baby's diapers? For the first few days after birth, the number of wet diapers typically increases each day. By the fifth day after birth, expect your baby to have at least six wet diapers a day and three or more bowel movements a day. The stool will be dark and sticky for the first couple of days, eventually becoming seedy, loose and golden yellow.
- Does your baby seem healthy? A baby who seems satisfied after feedings and is alert and active at other times is likely getting enough milk.
Trust your instincts
You know your baby best. If you sense something isn't right, contact your baby's doctor — especially if your baby:
- Isn't gaining weight
- Isn't wetting at least six diapers a day
- Isn't having regular bowel movements
- Passes urine that's deep yellow or orange
- Is consistently fussy after feedings
- Seems sleepy all the time
- Has yellow discoloration of the skin and eyes (jaundice)
- Spits up forcefully or more than a small amount at a time
Remember, every baby is unique and so are their feeding patterns. If you have questions about your baby's growth and development, talk to your baby's doctor.
-
Breastfeeding support
There's more you can do for your breastfeeding partner than you might realize. Understand how to provide breastfeeding support.
If your partner plans to breastfeed your new baby, your support can make all the difference. Understand what you can do to help.
How can I help my family prepare for breastfeeding?
You can start helping your partner prepare for breastfeeding by taking time to understand the benefits. Breast milk contains the right balance of nutrients for your baby and boosts your baby's immune system. It's considered the gold standard for infant nutrition.
The American Academy of Pediatrics recommends exclusive breastfeeding for the first six months after birth — and breastfeeding in combination with solid foods until at least age 1. Extended breastfeeding is recommended as long as your partner and your baby wish to continue.
To learn more about the benefits of breastfeeding, attend breastfeeding classes with your partner. If you know the basics of the techniques involved, you might be better able to help your partner after birth. These classes can also help you understand the impact that the use of bottles, pacifiers and supplemental feedings can have on the breastfeeding process, and spur you and your partner to make decisions together about how you'll care for your baby.
What can I do to support my breastfeeding partner?
To help your partner breastfeed:
- Provide encouragement. Your attitude toward breastfeeding might influence your partner's decision to continue breastfeeding. Tell your partner that you support her decision to breastfeed. Remind her that you appreciate the effort involved.
- Make her comfortable. When your partner is breastfeeding, offer her a pillow, a blanket, a drink of water or anything else she might like to have nearby.
- Get involved in feedings. Carry the baby to your partner. Afterward, burp the baby, change the baby's diaper or help the baby go back to sleep.
- Care for the baby. Offer to care for the baby, or other children at home, so that your partner can nap between feedings.
- Take on additional household responsibilities. Consider redividing your household tasks so that your partner has more time to rest.
- Stick around. Breastfeeding is a warm and loving activity. Sit nearby your partner and enjoy the moment together.
- Listen. Does your partner have breastfeeding concerns? If so, be a good listener. If necessary, encourage her to seek help from her healthcare provider or a lactation consultant.
What else can I do?
Your partner and your baby will develop a special bond during breastfeeding. At times you might feel envious of their connection. Remember that the bond between you and your baby is special and important, too.
Give your baby plenty of cuddles, hugs and skin-to-skin contact. Sing songs, take walks or play games that are special to just you and your baby. By spending time with your baby, you'll develop your own unique relationship.
-
Choosing a breast pump
Should you invest in an electric breast pump? A double pump? A lightweight pump? If you're in the market for a breast pump, ask yourself these questions and more.
Many breastfeeding mothers consider breast pumps as important as car seats and baby wipes. Whether you're going back to work or simply want the flexibility a breast pump can offer, you'll have many choices. Here's help deciding which type of breast pump is best for you.
How often will you use the breast pump?
If you'll be away from the baby only occasionally and your milk supply is well-established, a simple hand pump might be all you need. You simply place a cone-shaped shield on your breast and squeeze the handle to express the milk. If you're returning to work full time or you're planning to be away from your baby for more than a few hours a day, an electric pump is a better option.
Consider waiting to get a pump until after your baby is born, when you might better know how you'll be using it.
Will you need to pump as quickly as possible?
A typical pumping session lasts about 10 to 15 minutes a breast. If you'll be pumping at work or in other time-crunched situations, you might want to invest in an electric breast pump that allows you to pump both breasts at once. A double-breast pump helps stimulate milk production while reducing pumping time by half.
How much can you afford to spend on the pump?
You can buy breast pumps from medical supply stores and most drugstores and baby stores, as well as many discount department stores. Electric pumps typically cost more than manual models. Because there's a small risk of contamination, don't borrow or buy a used personal-use breast pump.
You might also consider renting a hospital-grade electric breast pump from a hospital or medical supply store — especially if you're pumping milk while your baby is hospitalized or you've chosen to feed your baby expressed milk rather than breastfeed your baby. If you rent a pump, you'll need to buy the equipment that attaches your breast to the pump (pumping kit).
Most health insurance plans cover the cost of buying or renting a breast pump.
Is the pump easy to assemble and transport?
If the breast pump is difficult to assemble, take apart or clean, it's bound to be frustrating — which might reduce your enthusiasm for pumping. Make sure you can remove any parts of the pump that come in contact with your skin or milk for cleaning after use.
If you'll be toting the pump to work every day or traveling with the pump, look for a lightweight model. Some breast pumps come in a carrying case with an insulated section for storing expressed milk. Also keep noise level in mind. Some electric models are quieter than others. If it's important to be discreet, make sure the pump's noise level is acceptable.
Is the suction adjustable?
What's comfortable for one woman might be uncomfortable for another. If you opt for an electric pump, choose one that allows you to control the degree of suction and cycling speed.
Are the breast shields the correct size?
Breast shields are the cone-shaped cups that fit over your breasts and nipples. If you're concerned that the standard breast shield will be too small, check with individual manufacturers about other options. Larger or replacement shields are often available. If you want to pump both breasts at once, make sure the pump is equipped with two breast shields.
What if the electricity fails?
An electric pump needs to be plugged in. If an outlet isn't accessible or the power fails, you'll need a rechargeable battery pack. In case of emergency, you might want to keep a manual pump handy.
If you're not sure which type of breast pump would be best for you, ask for help. A lactation consultant can help you make the best choice — and offer support as you start to use your breast pump or if you run into trouble. If you haven't worked with a lactation consultant, ask your baby's doctor for a referral or check with the obstetrics department at a local hospital.
-
Extended Breastfeeding
Curious about extended breastfeeding? Know the benefits, the role breast milk plays in an older baby's diet and how to handle others' opinions on the topic.
You've breastfed your baby for a year. Congratulations!
If you plan to breastfeed your baby beyond age 1 — also known as extended breastfeeding — you might have questions about the process. Get the facts about extended breastfeeding.
Is extended breastfeeding recommended?
The American Academy of Pediatrics recommends exclusive breastfeeding for the first six months after birth — and breastfeeding in combination with solid foods until at least age 1. Extended breastfeeding is recommended as long as you and your baby wish to continue.
What are the benefits of extended breastfeeding?
The benefits of extended breastfeeding for a baby include:
- Balanced nutrition. Breast milk is considered the gold standard for infant nutrition. As your baby gets older, the composition of your breast milk will continue to change to meet his or her nutritional needs. There's no known age at which breast milk is considered to become nutritionally insignificant for a child.
- Boosted immunity. As long as you breastfeed, the cells, hormones and antibodies in your breast milk will continue to bolster your baby's immune system.
- Improved health. Research suggests that the longer breastfeeding continues and the more breast milk a baby drinks, the better his or her health might be.
The benefits of extended breastfeeding for a mother include:
- Reduced risk of certain illnesses. Extended breastfeeding — as well as breastfeeding for 12 months or more cumulatively in life — has been shown to reduce the risk of breast cancer, ovarian cancer, rheumatoid arthritis, high blood pressure, heart disease and diabetes.
- Improved health. Research suggests that the longer breastfeeding continues and the more breast milk a baby drinks, the better a mother's health might be.
What role does breast milk play in an older baby's diet?
It depends on how much breast milk your baby is drinking.
After age 1, a baby might continue regularly drinking a moderate amount of breast milk. As a result, breast milk will continue to be a major source of nutrients for him or her. Other babies, however, might use solid foods to meet their nutritional needs and only want small amounts of breast milk.
If you have questions about your baby's diet or the role breast milk might play in it as he or she grows, talk to your baby's doctor or your healthcare provider.
Will extended breastfeeding make the weaning process more difficult?
Not necessarily.
It's often easiest to begin weaning when your baby initiates the process — which might be sooner or later than you expect.
Weaning often begins naturally at about age 6 months, when solid foods are typically introduced. Some babies begin to gradually transition from breast milk and seek other forms of nutrition and comfort closer to age 1. Others might not initiate weaning until their toddler years, when they become less willing to sit still during breastfeeding.
How should I handle negative reactions to extended breastfeeding?
Worldwide, babies are weaned on average between ages 2 and 4. In some cultures, breastfeeding continues until children are age 6 or 7. In other parts of the world, however, extended breastfeeding is less common and can sometimes provoke uninformed, negative reactions.
How long you breastfeed is up to you and your baby. If loved ones — and even strangers — share their opinions about when to wean, remind them that the decision is yours. Try not to worry about what other people think. Instead, trust your instincts.
Extended breastfeeding can be an intimate way to continue nurturing your baby. If you're considering extended breastfeeding, think about what's best for both you and your baby — and enjoy this special time together.
-
Pumping tips
Breastfeeding is a commitment — and your efforts are worthwhile. If you're pumping, follow simple tips for maintaining your milk supply, from pumping often to drinking plenty of fluids.
Breastfeeding is based on supply and demand. The more you breastfeed your baby — or pump while you're away from your baby — the more milk your breasts will produce. Consider seven tips for pumping success.
1. Relax
Stress can hinder your body's natural ability to release breast milk. Find a quiet place to pump. It might help to massage your breasts or use warm compresses. You might want to think about your baby, look at a picture of your baby or listen to relaxing music.
2. Pump often
The more you pump, the more milk you'll produce. If you're working full time, try to pump for 15 minutes every few hours during the workday. If you can, pump both breasts simultaneously. A double breast pump helps stimulate milk production while reducing pumping time by half.
3. When you're with your baby, breastfeed on demand
The more you breastfeed your baby when you're together, the greater your supply will be when you pump. Depending on your schedule, try more-frequent evening, early morning or weekend feedings. If you have a predictable schedule, you might ask your baby's caregivers to avoid feeding your baby during the last hour of care — so that you can breastfeed your baby as soon as you arrive.
4. Avoid or limit formula feedings
Formula feedings will reduce your baby's demand for breast milk, which will lower your milk production. To maintain your milk supply, it's important to pump anytime your baby has a feeding of formula or expressed breast milk.
Remember, the more you breastfeed your baby or pump while you're apart, the more milk you'll produce. You might also pump extra milk — either after or between breastfeeding sessions — and freeze it for future use.
5. Drink plenty of fluids
Water, juice and milk can help you stay hydrated. Limit soda, coffee and other caffeinated drinks, though. Too much caffeine might lead to irritability or interfere with your baby's sleep. If you choose to have an occasional alcoholic drink, avoid breastfeeding for two hours afterward.
6. Don't smoke
Smoking can reduce your milk supply, as well as change the taste of your milk and interfere with your baby's sleep. Secondhand smoke also is a concern. Secondhand smoke increases the risk of sudden infant death syndrome (SIDS), as well as respiratory illnesses. If you smoke, ask your doctor for options to help you quit. In the meantime, avoid smoking just before or during a feeding.
7. Take good care of yourself
Eat a healthy diet, including plenty of fruits, vegetables and whole grains. Include physical activity in your daily routine. Sleep when the baby sleeps — and don't be afraid to ask for help when you need it.
Also consider your birth control options. Breastfeeding itself isn't a reliable form of birth control, and birth control pills that contain estrogen can interfere with milk production. While you're breastfeeding, you might want to use condoms or other forms of birth control.
Breastfeeding is a commitment, and your efforts to maintain your milk supply are commendable. If you're having trouble maintaining your milk supply or you're concerned that you're not producing enough milk, ask your doctor or lactation consultant for other suggestions.
-
Weaning tips
Weaning: Tips for breastfeeding mothers Weaning doesn't have to be difficult. Find out how to choose the right time and what you can do to ease your child's transition to the bottle or cup.
If you're breastfeeding, you might have questions about weaning. When is the right time? Will weaning upset your child? How can you avoid engorgement? Get the facts about weaning and how you can make the process a more positive one for you and your child.
When's the best time to start weaning?
The American Academy of Pediatrics recommends exclusive breastfeeding for the first six months after birth — and breastfeeding in combination with solids foods until at least age 1. Extended breastfeeding is recommended as long as you and your baby wish to continue. Still, when to start weaning your child is a personal decision.
It's often easiest to begin weaning when your baby starts the process. Changes in breastfeeding patterns leading to eventual weaning often begin naturally at age 6 months, when solid foods are typically introduced. Some children begin to seek other forms of nutrition and comfort at around age 1. By this age, children typically eat a variety of solid foods and might be able to drink from a cup. Other children might not initiate weaning until they become toddlers, when they're less willing to sit still during breastfeeding.
You might also decide when to start the weaning process yourself. This might be more difficult than following your child's lead — but can be done with extra care and sensitivity.
Whenever you choose to start weaning your baby from the breast, stay focused on your child's needs as well as your own. Resist comparing your situation with that of other families, and consider rethinking any deadlines you might have set for weaning when you were pregnant or when your baby was a newborn.
Are there certain times when it wouldn't be smart to start weaning?
Consider delaying weaning if:
- You're concerned about allergens. Some research suggests that exclusive breastfeeding for at least six months — instead of using formula made with cow's milk — might prevent or delay eczema, cow's milk allergy, and wheezing in early childhood.
- Your child isn't feeling well. If your child is ill, postpone weaning until he or she is feeling better. You might also consider postponing weaning if you're not feeling well. You're both more likely to handle the transition well if you're in good health.
- A major change has occurred at home. Avoid initiating weaning during a time of major change at home. If your family has recently moved or your child care situation has changed, for example, postpone weaning until a less stressful time.
What's the best way to begin weaning?
Take it slow. Slowly tapering off how long and how often you breastfeed each day — over the course of weeks or months — will cause your milk supply to gradually diminish and prevent engorgement. If you experience engorgement during the weaning process, apply cold compresses to your breasts to help decrease swelling and discomfort.
Children tend to be more attached to the first and last feedings of the day, when the need for comfort is greater. These feedings might be the last ones your child drops. As a result, it might be easier to drop a midday breastfeeding session first. If you're weaning a child age 1 or older, consider not offering this feeding and seeing if he or she requests it. After a lunch of solid food, your child might become interested in an activity and naturally give up this session. Once you've successfully dropped one feeding, you can start working on dropping another.
You might also choose to wean your baby from breastfeeding and offer expressed breast milk in a cup during the day but continue breastfeeding at night. Remember, it's up to you and your child.
Should I refuse feedings during the weaning process?
Refusing to breastfeed when your child wants to nurse can backfire and increase your child's focus on the activity. If your child wants to nurse, nurse him or her. Then, continue working to distract him or her with new foods, activities and sources of reassurance — such as a favorite stuffed animal — around the times of your typical breastfeeding sessions. It might help to avoid sitting in your usual breastfeeding spots with your child during these times.
What about nutrition after weaning?
If you wean your child from breastfeeding before age 1, use expressed breast milk or iron-fortified formula. Ask your child's doctor to recommend a formula. Don't give your child cow's milk until after his or her first birthday.
You can wean your child to a bottle and then a cup or, if your child seems ready, directly to a cup. Keep in mind that if you wean your child to a bottle, you'll eventually have to wean him or her to a cup.
If you're introducing your child to a bottle for the first time, do so at a time when your child isn't extremely hungry and might have more patience. Choose a bottle nipple with a slow flow at first. If you use a bottle nipple with a fast flow, your child might become accustomed to that and get frustrated with the pacing and different flow rates of milk during breastfeeding.
How long does weaning take?
Depending on your approach, weaning could take days, weeks or months. Remember, however, that rushing the weaning process might be upsetting for your child and cause breast engorgement.
Breastfeeding is an intimate activity for you and your child. You might have mixed emotions about letting go. But by taking a gradual approach to weaning — and offering plenty of love and affection — you can help your child make a smooth transition to a bottle or cup.
Development
-
Child development
Every child grows and develops at his or her own pace. Still, child development tends to follow a fairly predictable path. Find out what language, social, cognitive and physical milestones to expect from ages 2 to 5.
Age 2
At age 2, your child might have completed these skills: Language skills.
- Speak at least 50 words. Link two words together, such as "my cup" or "no juice." Speak clearly enough for parents to understand about half of the words.
- Social skills. Show more independence. Become defiant. Copy others. Get excited when with other children.
- Cognitive skills. Play simple make-believe games. Begin to sort objects by shape and color. Find hidden objects.
- Physical skills. Stand on tiptoes. Begin to run. Kick a ball.
Age 3
At age 3, your child might have completed these skills:
- Language skills. Speak 250 to 500 words or more. Speak in three- and four-word sentences. Correctly use pronouns (I, you, me, mine). State his or her first name. Speak clearly enough for strangers to understand about 75 percent of the time.
- Social skills. Take turns. Express affection openly. Easily separate from parents. Get upset with major changes in routine.
- Cognitive skills. Turn book pages one at a time. Copy a circle. Do puzzles with three or four pieces.
- Physical skills. Walk up and down stairs, alternating feet. Climb, run and pedal a tricycle.
Age 4
At age 4, your child might have completed these skills:
- Language skills. Answer simple questions. Use sentences with four or more words.
- Social skills. Cooperate with other children. Talk about likes and dislikes. Become more creative with make-believe play.
- Cognitive skills. Print some capital letters. Draw a person with two to four body parts. Understand the idea of counting. Start to understand time.
- Physical skills. Hop or stand on one foot for two seconds. Catch a bounced ball most of the time. Use scissors with supervision.
Age 5
At age 5, your child might have completed these skills:
- Language skills. Understand rhyming. Use sentences that give many details. Use the future tense. State his or her full name.
- Social skills. Want to be like his or her friends. Can follow rules. Aware of gender. Like to sing, act and dance.
- Cognitive skills. Know about common items, such as food and money. Count 10 or more objects. Copy a triangle and other geometric patterns.
- Physical skills. Stand on one foot for at least 10 seconds. Hop, skip, swing and do somersaults. Use the toilet on his or her own.
If your child's development seems to be lagging behind in certain areas, share your concerns with your child's doctor.
-
Infant Development: Birth to 3 months
Infant development begins at birth. Consider major infant development milestones from birth to 3 months — and know what to do when something's not right.
A lot happens during your baby's first three months. Most babies reach certain milestones at similar ages, but infant development isn't an exact science. Expect your baby to grow and develop at his or her own pace. As you get to know your baby, consider these general infant development milestones.
What to expect
At first, caring for your baby might feel like an endless cycle of feeding, diapering and soothing. But soon, signs of your baby's growth and development will emerge.
- Motor skills. Your newborn's head will be wobbly at first and movements will be jerky. But soon your baby will be able to lift his or her head and chest while lying on his or her stomach, as well as stretch and kick his or her legs in that position. If you offer a toy, your baby might grasp it and hold on tight for a few moments.
- Hearing. Your infant will be sensitive to noise levels. Expect your baby to begin responding to the sound of your voice by smiling and gurgling back at you. He or she will also begin turning toward the direction of sounds.
- Vision. Your baby will probably focus on your face, particularly your eyes, during feedings. At age 1 month, your baby will prefer to look at bold patterns in sharply contrasting colors or black-and-white. By around age 2 months, your baby's eyes will become more coordinated, allowing for tracking an object. Soon your baby will begin to recognize familiar objects and people at a distance.
- Communication. By age 2 months, your baby might coo and repeat vowel sounds when you talk or gently play together.
Promoting your baby's development
Your relationship with your child is the foundation of his or her healthy development. Trust your ability to meet your baby's needs. You can:
- Hold your baby. This can help your newborn feel safe, secure and loved. Let your baby grasp your little finger and touch your face.
- Speak freely. Simple conversation lays the groundwork for language development. Sing. Read a story out loud. Ask questions and respond to your baby's coos and gurgles. Describe what you see, hear and smell around the house and when you're out and about. Remember that your tone of voice communicates ideas and emotions as well.
- Change positions. Hold your baby facing outward. With close supervision, place your baby on his or her tummy to play. Hold a colorful toy or make an interesting noise to encourage your baby to pick up his or her head. Many newborns get fussy or frustrated on their tummies, so keep these sessions brief at first — just a few minutes at a time. If drowsiness sets in, place your baby on his or her back to sleep.
- Respond quickly to tears. For most newborns, crying spells peak about six weeks after birth and then gradually decline. Whether your baby needs a diaper change, feeding session or simply warm contact, respond quickly. Don't worry about spoiling your baby with too much attention. Your care will help build a strong bond with your baby — and the confidence he or she will need to settle down without your help one day.
When something's not right
Your baby might reach some developmental milestones ahead of schedule and lag behind on others. This is normal. It's a good idea to be aware of the warning signs of developmental delay, however. Consult your baby's doctor if you're concerned about your baby's development or you notice any of these red flags by age 3 months:
- Hasn't shown any improvement in head control
- Doesn't seem to respond to loud sounds
- Doesn't smile at people or the sound of your voice
- Doesn't follow moving objects with his or her eyes
- Doesn't notice his or her hands
- Doesn't grasp and hold objects
Remember that every baby is unique — but your instincts are important, too. The earlier a problem is detected, the earlier it can be treated.
-
Infant development: 4 to 6 months
From ages 4 to 6 months, your baby becomes more aware of his or her surroundings. Infant development milestones include rolling over, clapping hands and babbling.
The newborn days are behind you. As your baby becomes more alert and mobile, each day will bring exciting new adventures. Every experience — from cuddling before nap time to listening to a sibling's chatter — will help your baby learn more about the world.
Expect your baby to grow and develop at his or her own unique pace. Consider these general infant development milestones as your baby's strengths and preferences begin to emerge.
What to expect
As your baby becomes more aware of the surrounding world, he or she will begin exploring. From ages 4 to 6 months, your baby is likely to enjoy:
- Evolving motor skills. Your baby's arms and legs probably wiggle and kick more purposefully now. Soon you might notice your baby rocking on his or her stomach and eventually rolling over. As your baby gains muscle strength, he or she will have better head control. Most babies this age raise their heads when lying facedown. They might even try to push themselves up or bear weight on their legs. Around age 6 months, many babies begin sitting alone after being positioned upright.
- Improving hand-eye coordination. Your baby will probably grasp your finger, a rattle or a soft object. Anything within reach is likely to end up in your baby's mouth. You might notice your baby pulling objects closer with a raking motion of the hands.
- Clearer vision. Your baby is beginning to be able to distinguish subtle shade of reds, blues and yellows. He or she might enjoy more complex patterns and shapes. You might notice your baby concentrating on a toy or staring at his or her reflection. If you roll a ball across the floor, your baby will probably turn his or her head to follow the action.
- Babbling and other new sounds. Babies this age often start to babble chains of consonants. Your baby might respond to sound by making sounds and use his or her voice to express joy. He or she also might distinguish emotions by tone of voice — and begin responding to "no." Your baby might even recognize his or her name.
Promoting your baby's development
At this age, learning and play are inseparable. It doesn't take expensive educational toys or intense effort, however, to capture your baby's attention. To promote infant development:
- Talk to your baby. Ask questions and respond to your baby's coos and gurgles. Describe what you see, hear and smell around the house, outdoors, and when you're out and about. Use simple words such as "baby," "cat," "go," "walk," "hot" and "cold." Remember that your tone of voice and facial expression can communicate ideas and emotions.
- Change positions. Lay your baby on his or her tummy for a few supervised minutes. Hold a colorful toy or make a noise to encourage your baby to pick up his or her head or practice rolling over. Hold your baby's hands while he or she is lying down and say, "Are you ready to stand up? Here we go!" Count to three as you gently pull your baby to a standing position. When your baby's ready, try a sitting position. Hold your baby or use pillows for support.
- Offer simple toys. Babies this age often enjoy colorful toys, especially those that make sounds. Try a musical toy, a rattle with a handle, a soft ball or a wooden spoon. To help your baby focus, put out only one or two toys at a time. Place one toy slightly out of reach to encourage your baby to stretch and creep. Shake a rattle behind your baby's head and let him or her turn and grab it. Let your baby watch his or her movements in a mirror.
- Read to your baby. Reading to a baby promotes speech and thought development. Your baby will soak in your words and might even mimic the sounds you make. Start with books featuring large, brightly colored pictures. Describe what's happening on each page. Point to and name common objects.
- Play favorite games. Cover your face with your hands, then remove your hands and say, "Peekaboo, I see you!" Play patty-cake. Ask, "Where are your toes?" Then touch your child's toes and say, "Here are your toes!" Hide one of your baby's toys with the corner of a blanket and encourage him or her to find it.
- Take time to cuddle. Balance stimulation with plenty of quiet time. Gentle caresses and tender kisses can help your baby feel safe, secure and loved. When you hold or rock your baby, talk quietly or sing soothing songs.
- Turn on the tunes. Music can help calm, entertain and teach your baby. Sing or play lullabies, upbeat children's songs or your own favorites.
- Let your baby set the pace. When your baby turns away, closes his or her eyes, or gets fussy, take a break. Even babies need space. Get to know your baby's unique personality, temperament, likes and dislikes. Responding to your baby's needs will help you continue to build your baby's trust in you.
When something's not right
Your baby might reach some developmental milestones ahead of schedule and lag behind a bit on others. This is normal. It's a good idea, however, to be aware of the signs or symptoms of a problem.
Consult your baby's doctor if you're concerned about your baby's development or your baby:
- Has very stiff or tight muscles
- Seems extremely floppy
- Reaches with only one hand
- Hasn't shown any improvement in head control
- Doesn't respond to sounds, such as by startling to sudden loud noises
- Doesn't reach for or bring objects to his or her mouth
- Doesn't attempt to roll over or sit
- Has an eye or eyes that consistently turn in or out
- Doesn't babble
- Doesn't seem to enjoy being around people or spontaneously smile
Trust your instincts. The earlier a problem is detected, the earlier it can be treated. Above all, delight in your baby's discoveries and abilities.
-
Infant Development: 7 to 9 Months
Your baby might surprise you with how quickly he or she is picking up new skills. Infant development milestones for a 7- to 9-month-old include sitting, standing and laughing.
As your baby becomes more mobile and inquisitive, infant development takes off. It might seem that your baby learns something new every day. Understand your baby's next milestones and what you can do to promote his or her growth.
What to expect
Your baby will continue to grow and develop at his or her own pace. From ages 7 to 9 months, your baby is likely to experience:
- Advancing motor skills. By this age, most babies can roll over in both directions — even in their sleep. Some babies can sit on their own, while others need a little support. You might notice your baby beginning to scoot, rock back and forth, or even crawl across the room. Some babies this age can pull themselves to a standing position. Soon your baby might cruise along the edge of the couch or coffee table.
- Improved hand-eye coordination. Most babies this age transfer objects from one hand to another or directly to their mouths. Pulling objects closer with a raking motion of the hands will give way to more-refined movements, such as picking up objects with just the thumb and forefinger. This improving dexterity will help your baby handle a spoon and soft finger foods.
- Evolving communication. Your baby will communicate with you through sounds, gestures and facial expressions. You'll probably hear plenty of laughing and squealing. Some babies might repeat the sounds they hear — or give it their best shot. Your baby's babbling is likely to include chains of sounds, such as "ba-ba-ba." You might even pick out an occasional "mama" or "dada."
- Stranger anxiety. Many babies this age become wary of strangers. Your baby might resist staying with anyone other than you. If your baby fusses when you leave, have the person staying with your child create a distraction. Then say goodbye with a hug and kiss and a reminder that you'll be back soon. Your baby will likely stop crying as soon as you're out of sight.
- Teething. You can expect the first tooth anytime. You might notice your baby drooling more than usual and chewing on just about anything. Try gently rubbing the gums with one of your fingers or offer a rubber teething ring. When your baby's first teeth appear, use a soft-bristled toothbrush to clean them twice a day. Until your child learns to spit — at about age 3 — use a smear of fluoride toothpaste no bigger than the size of a grain of rice.
Promoting your baby's development
For babies of any age, learning and play are inseparable. To support your budding adventurer:
- Create an exploration-safe environment. Keep only safe objects within your baby's reach. Move anything that could be poisonous, pose a choking hazard or break into small pieces. Cover electrical outlets, use stairway gates, place cords from blinds or shades out of reach, and install child locks on doors and cabinets. If you have furniture with sharp edges, remove it from rooms where your baby plays. The same goes for lightweight objects your baby can use to pull himself or herself to a standing position, such as plant stands, decorative tables, potted trees and floor lamps. Anchor bookcases, televisions and their stands to the wall.
- Keep chatting. You've likely been talking to your baby all along. Keep it up! Narrate what you're doing, and give your baby time to respond. Say something to your baby and then wait for him or her to repeat the sounds. Sing simple songs. Ask your baby questions that involve more than a yes or no response. You might not be able to pick words from your baby's babble, but you can encourage a back-and-forth conversation.
- Teach cause and effect. Push the button on a musical toy and dance to the tune. Open the door on a toy barn and listen to the cow say "moo." Help your baby do the same. Self-confidence will grow as your baby realizes he or she can make things happen.
- Take time to play. By now, you and your baby might be old pros at classics, such as peekaboo, patty-cake and itsy-bitsy spider. Get creative. Arrange cushions and pillows on a carpeted floor and encourage your baby to creep or crawl over them. Stack blocks and invite your baby to knock them down. If you're up for a mess, smear applesauce on the highchair tray and let your baby "paint" with the mixture. At bath time, provide small containers and plastic utensils for pouring and mixing.
- Pull out the books. Set aside time for reading every day — even if it's only a few minutes. Reading aloud is one of the simplest ways to boost your baby's language development. Make it more interesting with facial expressions, sound effects and voices for various characters. Store books within easy reach so that your baby can explore them whenever the mood strikes.
When something's not right
Your baby might reach some developmental milestones ahead of schedule and lag behind a bit on others. This is normal. It's a good idea, however, to be aware of the signs or symptoms of a problem.
Consult your baby's doctor if you're concerned about your baby's development or your baby:
- Doesn't roll over in either direction or sit with help
- Doesn't bear some weight on legs
- Doesn't try to attract attention through actions
- Doesn't babble
- Shows no interest in games of peekaboo
Trust your instincts. The earlier a problem is detected, the earlier it can be treated. Then you can set your sights on the milestones that lie ahead.
-
Infant Development: 10 to 12 months
Your baby will keep you on your toes in the next few months. Infant development milestones for a 10- to 12-month-old include crawling and improved hand-eye coordination.
Your baby is constantly on the move. Nothing makes him or her happier than dropping a spoon from the highchair over and over again. If you aren't stifling the urge to say "No!" chances are you've said it in the last few hours. Welcome to life with a 10- to 12-month-old! At this age, infant development is rapid.
What to expect
From ages 10 to 12 months, your baby is likely to enjoy:
- Improved motor skills. Most babies this age can sit without help and pull themselves to a standing position. Creeping, crawling and cruising along the furniture will eventually lead to walking. By 12 months, your baby might take his or her first steps without support.
- Better hand-eye coordination. Most babies this age can feed themselves finger foods, grasping items between the thumb and forefinger. Your baby might delight in banging blocks together, placing objects in a container and taking them out, as well as poking things with his or her index finger.
- Evolving language. Most babies this age respond to simple verbal requests. Your baby might become skilled at various gestures, such as shaking his or her head no or waving bye-bye. Expect your baby's babbling to take on new inflection and evolve to words such as "dada" and "mama." You might hear certain exclamations, such as "uh-oh!"
- New cognitive skills. As your baby's understanding of object permanence improves, he or she will be able to easily find hidden objects. Although your leaving the room might lead to crying, your baby will begin to realize that you still exist even when you're out of sight. You might find your baby imitating you by brushing his or her hair, pushing buttons on the remote control or "talking" on the phone.
Promoting your baby's development
Your baby's budding curiosity is bound to keep you on your toes. Keep your baby safe while challenging him or her to learn through play.
- Create an exploration-safe environment. Move anything that could be poisonous, pose a choking hazard or break into small pieces from your baby's reach. Cover electrical outlets, use stairway gates, and install child locks on doors and cabinets. If you have furniture with sharp edges, pad the corners or remove it from areas where your baby plays. The same goes for lightweight objects your baby might use to pull himself or herself to a standing position, such as plant stands and decorative tables. Anchor bookcases, televisions and their stands to the wall.
- Snuggle up and read. Set aside time for reading every day — even if it's only a few minutes. At this age, your baby might love books with flaps, textures or activities. Make your reading more interesting by adding facial expressions, sound effects and voices for characters. Store books within easy reach so that your baby can explore them whenever the mood strikes.
- Keep conversations going. If your baby reaches for a book, ask, "Would you like to read a story?" If he or she points to the cow on the cover, say, "You found the cow! What does a cow say?" Wait for your baby's response and then offer the correct answer. As you're reading the book, get creative. Make up your own stories to fit the pictures. Ask your baby questions about the pictures. Don't limit yourself to yes or no questions.
- Help your baby handle his or her feelings. Expect episodes of frustration as your baby struggles to make sense and take control of his or her environment. If your baby throws plastic rings out of frustration, calmly pick up the pieces and say, "I can see you're frustrated. Let's figure it out. The big ring goes here. Now you try." For some babies, learning a few words in sign language can be helpful. Teach your baby simple motions for common words, such as milk and blanket.
- Set limits. Babies don't have a sense of right or wrong. Praise your baby for good choices while steering him or her away from hazardous situations. Use a calm no if your baby hurts others. Explain calmly why the behavior isn't OK, and then redirect your baby's attention.
When something's not right
Your baby might reach some developmental milestones ahead of schedule and lag behind a bit on others. This is normal. It's a good idea, however, to be aware of the signs or symptoms of a problem.
Consult your baby's doctor if you're concerned about your baby's development or your baby:
- Doesn't crawl or consistently drags one side of the body while crawling
- Can't stand with help
- Doesn't use gestures, such as waving or shaking the head
- Doesn't babble or attempt words such as "mama" or "dada"
- Doesn't search for objects that are hidden while he or she watches
- Doesn't point to objects or pictures
Trust your instincts. The earlier a problem is detected, the earlier it can be treated. Then you can look forward to the delights and challenges that lie ahead.
-
Language Development
A baby's first words are music to a parent's ears. But how can you tell if your child's speech and language development is on track?
While every child learns to speak at his or her own pace, general milestones can serve as a guide to normal speech and language development — and help doctors and other health professionals determine when a child might need extra help.
By the end of 3 months
By the end of three months, your child might:
- Smile when you appear
- Make "cooing" sounds
- Quiet or smile when spoken to
- Seem to recognize your voice
- Cry differently for different needs
By the end of 6 months
By the end of six months, your child might:
- Make gurgling sounds when playing with you or left alone
- Babble and make a variety of sounds
- Use his or her voice to express pleasure and displeasure
- Move his or her eyes in the direction of sounds
- Respond to changes in the tone of your voice
- Notice that some toys make sounds
- Pay attention to music
By the end of 12 months
By the end of 12 months, your child might:
- Try imitating speech sounds
- Say a few words, such as "dada," "mama" and "uh-oh"
- Understand simple instructions, such as "Come here"
- Recognize words for common items, such as "shoe"
- Turn and look in the direction of sounds
By the end of 18 months
By the end of 18 months, your child might:
- Recognize names of familiar people, objects and body parts
- Follow simple directions accompanied by gestures
- Say as many as eight to 10 words
By the end of 24 months
By the end of 24 months, your child might:
- Use simple phrases, such as "more milk"
- Ask one- to two-word questions, such as "Go bye-bye?"
- Follow simple commands and understand simple questions
- Speak at least 50 words
When to check with your child's doctor
Talk to your child's doctor if your child hasn't mastered most of the speech and language development milestones for his or her age or you're concerned about any aspect of your child's development. Speech delays occur for many reasons, including hearing loss and developmental disorders. Depending on the circumstances, your child's doctor might refer your child to a hearing specialist (audiologist) or a speech-language pathologist.
In the meantime, talk to your child about what you're doing and where you're going. Sing songs and read together. Teach your child to imitate actions, such as clapping, and to say animal sounds. Practice counting. Show your child that you're pleased when he or she speaks. Listen to your child's sounds and repeat them back to him or her. These steps can encourage your child's speech and language development.
Health
-
Acetaminophen and children: Why dose matters
An acetaminophen overdose is serious — and it can happen easier than you might think. Here's how to protect your child.
Acetaminophen (Tylenol, others) has long been a standard remedy for fever and pain in children. It's effective and available without a prescription. But, in excess, it can be harmful. Here's what you need to know about acetaminophen overdoses and children.
What might cause an acetaminophen overdose?
An acetaminophen overdose can happen in the blink of an eye. Consider these scenarios:
- You're in a hurry. You might unknowingly give your child too much acetaminophen if you misread the instructions, don't carefully measure the medication, give two doses too close together — or if you don't realize that another caregiver has already given your child a dose.
- You combine medications. If your child has various cold symptoms, your instinct might be to combine acetaminophen with a cold remedy. This can be dangerous, however, because many cold medications already contain acetaminophen. Also, cough and cold medicines should be avoided in children younger than age 6 due to possibly serious side effects.
- You use the wrong formulation. You might cause an overdose if you give your child adult acetaminophen instead of a children's formulation.
- You decide that more is better. If you're not satisfied with the performance of the recommended dose of acetaminophen, you might increase the dose or its frequency and cause an accidental overdose.
- Your child mistakes the medication for candy or juice. Overdoses often occur when a child mistakes acetaminophen for something safe to eat or drink. This can happen when an adult leaves the bottle open or accessible after using medication.
What are the recommended acetaminophen doses?
If you give your child acetaminophen, read the product label carefully to determine the correct dose based on your child's weight. Generally, doses can be repeated every four hours, but shouldn't be given more than five times in 24 hours.
What happens if the acetaminophen dose is too much?
Too much acetaminophen overloads the liver's ability to process the drug safely. An acetaminophen overdose can lead to life-threatening liver problems.
If you're concerned about a possible acetaminophen overdose or notice early signs or symptoms of an overdose — nausea, vomiting, lethargy and abdominal pain within 24 hours — call a poison control center at 800-222-1222 in the United States or seek emergency care. If possible, note the strength or concentration of acetaminophen in the product to help poison control or the emergency responders assess your child. If you seek medical help, take the medication bottle with you.
In the hospital, a child with an acetaminophen overdose will have a blood test to determine if the concentration in his or her blood is toxic. If necessary, an antidote might be given to reverse the effects of the acetaminophen.
How can an acetaminophen overdose be prevented?
Before you give your child acetaminophen, consider whether he or she needs it. For example, the main goal of treating a child who has a fever is to improve his or her comfort — not to normalize his or her body temperature. In addition:
- Know your child's weight. Follow the directions and weight-based dose recommendations printed on medication labels.
- Use the measuring device that comes with your child's medication. Don't use household teaspoons — which can vary in size — to measure liquid acetaminophen. Don't give your child acetaminophen when he or she is taking other medications containing acetaminophen.
- Don't give your child adult formulations of acetaminophen.
- Securely replace child-resistant caps after using medication and store all medication in its original container out of your child's reach.
Careful use of acetaminophen and prompt treatment in case of an overdose can help prevent a tragedy.
-
Antidepressants for children and teens
Learn why antidepressants have warnings about suicidal thinking in children and teens, what to do before your child starts taking an antidepressant, and the warning signs of a potential problem.
Antidepressant drugs are often an effective way to treat depression and anxiety in children and teenagers. However, antidepressant use in children and teens must be monitored carefully, as rarely there can be severe side effects.
Antidepressants carry a Food and Drug Administration (FDA) black box warning about a risk of increased suicidal thinking and behavior in some individuals under the age of 25.
Although at first you may find the suicide warnings alarming, it's important to get the facts. Find out what the warnings mean and ask about all treatment options. This will help you make an informed decision about your child's health and weigh the benefits and risks of treatment options with your child's doctor.
Why do antidepressants have warnings about suicidal behavior in children?
The FDA reported that an extensive analysis of clinical trials showed that antidepressants may cause or worsen suicidal thinking or behavior in a small number of children and teens. The analysis showed that children and teens taking antidepressants had a small increase in suicidal thoughts, compared with those taking a sugar pill (placebo).
None of the children in any of the studies actually took his or her own life. Still, the FDA considered the findings concerning enough to issue a public health advisory and require manufacturers to label antidepressants with strong warnings about the link to suicidal thinking and behavior in children, adolescents and young adults ages 18 through 24.
However, not all mental health researchers believe these warnings are necessary. Newer research indicates that the benefits of antidepressants may be greater than the risk of suicide. And some research indicates that suicide rates in children decrease when they take antidepressants.
Which antidepressants must have the warnings about suicide?
Although the FDA analysis examined only nine antidepressants, the FDA extended the warning to all prescription antidepressants. This black box warning is the strongest safety warning that the FDA can issue about a prescription drug. The warning is printed in bold type framed in a black border at the top of the paper inserts that come with antidepressants.
How can medication meant to help treat depression and other illnesses lead to suicidal behavior in children?
Because of the risk of suicide from depression, it's difficult to establish a clear causal relationship between antidepressant use and suicide. Researchers speculate about a variety of potential reasons for an increased risk. In some children, antidepressants may also trigger anxiety, agitation, hostility, restlessness or impulsive behavior. These effects may indicate that the child's depression is getting worse or that the child is starting to develop suicidal thoughts.
Should children be treated with antidepressants at all?
The warnings about a possible link between antidepressants and suicidal thoughts do not mean that antidepressants should not be used in children. Nor are the warnings meant to frighten people away from antidepressants. However, the warnings should be taken as a caution to carefully weigh the pros and cons of using antidepressants in children and teenagers against the real risk of suicide as a result of untreated depression.
For many children and teens, antidepressants are an effective way to treat depression, anxiety, obsessive-compulsive disorder or other mental health conditions. If these conditions aren't treated effectively, your child may not be able to lead a satisfying, fulfilled life or do normal, everyday activities.
What should you do before your child starts taking an antidepressant?
It's important that your child have a thorough evaluation before he or she starts taking an antidepressant. A psychiatric evaluation by a psychiatrist — or a pediatrician or family physician who is experienced in the treatment of child and adolescent mood disorders — should include:
- A detailed review of any potential risk factors your child may have that increase the risk of self-harm
- An assessment of whether your child may have other mental illnesses, such as anxiety disorders, attention-deficit/hyperactivity disorder or bipolar disorder
- An evaluation of whether there's a family history of mental illnesses or suicide
Which antidepressants can children take?
The FDA has approved certain antidepressants for use in children and teenagers for different types of diagnoses. Antidepressants come with a medication guide that advises parents and caregivers about risks and precautions. Be sure to carefully read the medication guide and package insert, and discuss any questions with the prescribing physician and your pharmacist.
FDA-approved antidepressants for children and teenagers
Medication* Age (in years) Diagnosis Clomipramine (Anafranil) 10 and older Obsessive-compulsive disorder (OCD) Duloxetine (Cymbalta) 7 and older Generalized anxiety disorder Escitalopram (Lexapro) 12 and older Major depressive disorder Fluoxetine (Prozac) 8 and older 7 and older Major depressive disorder OCD Fluvoxamine 8 and older OCD Olanzapine and fluoxetine, combination drug (Symbyax) 10 and older Bipolar depression Sertraline (Zoloft) 6 and older OCD *Many of these drugs are also available in generic form. Recommended initial dose and maximum dose vary by age.
Physicians may use their medical judgment to prescribe other antidepressants for children for what's called off-label use. This is a clinically common practice for many types of medications for both children and adults.
What should you do once your child starts taking an antidepressant?
The FDA advises that doctors prescribe the smallest quantity of pills possible to help reduce the risk of deliberate or accidental overdose. Careful monitoring by parents, caregivers and healthcare professionals is important for any child or teenager taking an antidepressant for depression or any other condition.
The highest risk of suicidal thinking and behavior occurs:
- During the first few months of treatment with an antidepressant
- When the dosage is increased or decreased
Parents and caregivers should closely observe the child on a daily basis during these transition periods and watch for worrisome changes for the whole time the child takes antidepressants.
The FDA also recommends that your child receive close monitoring by his or her healthcare professional during the first few months of treatment. Frequency of contact with doctors or mental health professionals depends on your child's needs. Make sure you stick to your child's recommended appointment schedule.
What warning signs should you watch for when your child is taking antidepressants?
Sometimes the signs and symptoms of suicidal thoughts or self-harm are difficult to see, and your child may not directly tell you about such thoughts. Here are some signs that your child's condition may be worsening or that he or she may be at risk of self-harm:
- Talk of suicide or dying
- Attempts to commit suicide
- Self-injury
- Agitation or restlessness
- New or worsening anxiety or panic attacks
- Irritability
- Increasing sadness or worsening of depression symptoms
- Impulsiveness
- Extreme increase in talking, energy or activity
- Aggression, violence or hostility
- Trouble sleeping or worsening insomnia
- Spending more time alone
Contact your child's healthcare professional right away if any of these signs occur, if they get worse, or if they worry you, your child, a teacher or other caregiver.
Make sure your child doesn't stop antidepressant treatment without the guidance of the prescribing doctor. Suddenly stopping an antidepressant may cause flu-like symptoms or side effects referred to as discontinuation syndrome.
What other treatment options are available for children with depression?
Most children who take antidepressants for depression will improve with medication. However, combining medication with talk therapy (psychotherapy) is likely to be even more effective. Many types of psychotherapy may be helpful, but cognitive behavioral therapy and interpersonal therapy have been scientifically studied and shown to be effective for treating depression.
- Cognitive behavioral therapy. In cognitive behavioral therapy, a mental health professional can help your child improve coping skills, communication and problem-solving skills. Your child can also learn how to become aware of harmful ideas and behaviors, replace them with positive approaches, and manage emotions.
- Interpersonal therapy. With a focus on relationships, this therapy may help your teenager adapt to changes in current relationships and develop new ones.
For some children and teenagers with mild symptoms, talk therapy alone may be beneficial.
-
Baby's Head Shape: What's Normal?
A baby's head is easily molded. Know why and how to care for flat spots.
Many newborns have slightly uneven heads. But is it cause for worry? Understand what causes unevenness in babies' heads and when treatment is needed.
What causes a baby's head shape to appear uneven?
Sometimes a baby's head is molded unevenly while passing through the birth canal. In other cases, head shape changes after birth as a result of pressure on the back of the head when the baby lies on his or her back.
You'll notice two soft areas at the top of your baby's head where the skull bones haven't yet grown together. These spots, called fontanels, allow a baby's relatively large head to move through the narrow birth canal. They also accommodate your baby's rapidly growing brain during infancy.
Because your baby's skull is malleable, however, a tendency to rest the head in the same position can result in an uneven head shape well past the time when birth-related lopsidedness evens out. This is known as positional plagiocephaly.
What's normal and what isn't?
Your baby's doctor will check the soft spots on your baby's head and the shape of your baby's head at birth and at each well-baby exam — usually every two to four months for the first year.
Positional molding might be most noticeable when you're looking at your baby's head from above. From that view, the back of your baby's head might look flatter on one side than on the other. The cheekbone on the flat side might protrude, and the ear on the flat side might look pushed forward.
Is an uneven head shape cause for worry?
Your baby's head shape will most likely even out on its own. Positional molding is generally considered a cosmetic issue. Flat spots related to pressure on the back of the head don't cause brain damage or interfere with a baby's growth and development.
Keep in mind that if you spend too much time worrying about your baby's head shape, you might miss some of the fun of being a new parent. In a few short months, better head and neck control will help your baby keep pressure more evenly distributed on the skull.
How is an uneven head shape treated?
Your baby's head shape will most likely even out on its own. But changes in the way you position your baby can minimize unevenness and hasten its resolution. For example:
- Change direction. Continue to place your baby on his or her back to sleep, but alternate the direction your baby's head faces when you place him or her in the crib. Or place your baby's head near the foot of the crib one day, the head of the crib the next. You might also hold your baby with alternate arms at each feeding. If your baby returns to the original position while sleeping, adjust his or her position next time.
- Hold your baby. Holding your baby when he or she is awake will help relieve pressure on your baby's head from swings, carriers and infant seats.
- Try tummy time. With close supervision, place your baby on his or her tummy to play. Make sure the surface is firm.
- Get creative. Position your baby so that he or she will have to turn away from the flattened side of the head to look at you or to track movement or sound in the room. Move the crib occasionally to give your baby a new vantage point. Never rest your baby's head on a pillow or other type of soft bedding.
Helmets and head shape
If unevenness doesn't improve by age 4 months, your baby's doctor might prescribe a molded helmet to help shape your baby's head. The helmet provides guided growth, maintaining contact with the baby's head in all areas except for the flat spot.
Molded helmets are most effective when treatment begins by ages 4 to 6 months, when the skull is still malleable and the brain is growing rapidly. To be effective, the helmet must be worn 23 hours a day during the treatment period — often a number of months. The helmet is adjusted regularly — sometimes weekly — as the baby's head grows and changes shape. Treatment with a molded helmet isn't likely to be effective after age 1, when the skull bones are fused together and head growth becomes less rapid.
Recent research, however, suggests that repositioning with or without physical therapy might be as effective as helmet therapy in many cases.
Beyond positional molding
Sometimes an underlying muscular issue — such as torticollis — causes a baby to hold his or her head tilted to one side. In this case, physical therapy is important to help stretch the affected muscles and allow the baby to more freely change head positions.
Rarely, two or more of the bony plates in a baby's head fuse prematurely. This rigidity pushes other parts of the head out of shape as the brain grows. This condition, known as craniosynostosis, is typically treated during infancy. To give the brain enough space to grow and develop, the fused bones must be surgically separated.
Remember, most cases of unevenness in babies' head shapes will resolve on their own. If you're concerned about your baby's head shape, check with your baby's doctor.
-
Childhood vaccines
Do vaccines cause autism? Is it OK to skip certain vaccines? Get the facts on these and other common questions.
Childhood vaccines protect children from a variety of serious or potentially fatal diseases, including diphtheria, measles, polio and whooping cough (pertussis). If these diseases seem uncommon — or even unheard of — it's usually because these vaccines are doing their job.
Still, you might wonder about the benefits and risks of childhood vaccines. Here are straight answers to common questions about childhood vaccines.
Is natural immunity better than vaccination?
A natural infection might provide better immunity than vaccination — but there are serious risks. For example, a natural chickenpox (varicella) infection could lead to pneumonia. A natural polio infection could cause permanent paralysis. A natural mumps infection could lead to deafness. A natural Haemophilus influenzae type b (Hib) infection could result in permanent brain damage. Vaccination can help prevent these diseases and their potentially serious complications.
Do vaccines cause autism?
Vaccines do not cause autism. Despite much controversy on the topic, researchers haven't found a connection between autism and childhood vaccines. In fact, the original study that ignited the debate years ago has been retracted.
Are vaccine side effects dangerous?
Any vaccine can cause side effects. Usually, these side effects are minor — low-grade fever, fussiness and soreness at the injection site. Some vaccines cause a temporary headache, fatigue or loss of appetite. Rarely, a child might experience a severe allergic reaction or a neurological side effect, such as a seizure. Although these rare side effects are a concern, the risk of a vaccine causing serious harm or death is extremely small. The benefits of getting a vaccine are much greater than the possible side effects for almost all children.
Of course, vaccines aren't given to children who have known allergies to specific vaccine components. Likewise, if your child develops a life-threatening reaction to a particular vaccine, further doses of that vaccine won't be given.
Why are vaccines given so early?
The diseases that childhood vaccines are meant to prevent are most likely to occur when a child is very young and the risk of complications is greatest. That makes early vaccination — sometimes beginning shortly after birth — essential. If you postpone vaccines until a child is older, it might be too late.
Is it OK to pick and choose vaccines?
In general, skipping vaccines isn't a good idea. This can leave your child vulnerable to potentially serious diseases that could otherwise be avoided. And consider this: For some children — including those who can't receive certain vaccines for medical reasons — the only protection from vaccine-preventable diseases is the immunity of the people around them. If immunization rates drop, vaccine-preventable diseases might once again become common threats.
If you have reservations about particular vaccines, discuss your concerns with your child's doctor. If your child falls behind the standard vaccines schedule, ask the doctor about catch-up immunizations.
-
Cold Medicines for Kids
Cough and cold medicines can pose serious risks for young children. Know the facts and understand treatment alternatives.
Over-the-counter cough and cold medicines are the best way to help a child who has a cold feel better — right? Think again. Here's practical advice from Mayo Clinic.
What's the concern about cough and cold medicines for kids?
Over-the-counter cough and cold medicines are intended to treat the symptoms of coughs and colds, not the underlying disease. Research suggests that these medicines haven't been proved to work any better than inactive medicine (placebo). More important, these medications have potentially serious side effects, including fatal overdoses in children younger than 2 years old.
Don't use over-the-counter medicines, except for fever reducers and pain relievers, to treat coughs and colds in children younger than 6 years old. Also, consider avoiding use of these medicines for children younger than 12 years old.
What about antibiotics?
Antibiotics can be used to combat bacterial infections but have no effect on viruses, which cause colds. If your child has a cold, antibiotics won't help. Remember, the more your child uses antibiotics, the more likely he or she is to get sick with an antibiotic-resistant infection in the future.
Can any medications help treat the common cold?
An over-the-counter pain reliever — such as acetaminophen (Tylenol, others) or ibuprofen (Advil, Children's Motrin, others) — can reduce a fever and ease the pain of a sore throat. However, fevers are generally harmless. The main purpose for treating them is to help your child feel comfortable.
If you give your child a pain reliever, follow the dosing guidelines carefully. For children younger than 3 months old, don't give acetaminophen until your baby has been seen by a doctor. Don't give ibuprofen to a child younger than 6 months old or to children who are vomiting constantly or are dehydrated. Also, use caution when giving aspirin to children.
Is codeine OK?
No. The Food and Drug Administration has issued its strongest warning against the use of codeine to treat a cough or pain and the narcotic tramadol (Ultram) to treat pain in children younger than 12 years old. This is due to the potential for serious side effects, such as slowed or difficult breathing.
How can I help my child feel better?
To help your child cope with a cough or cold:
- Offer fluids. Liquids such as water, juice and broth might help thin secretions. Warm liquids, such as tea or chicken soup, might have a soothing effect, increase the flow of nasal mucus and loosen respiratory secretions.
- Run a cool-mist humidifier. This can help shrink nasal passages and loosen nasal secretions.
- Use a suction bulb. Use this device on a baby or young child to draw mucus out of the nose.
- Use nasal saline. Over-the-counter saline can keep nasal passage moist. In younger children, use saline nasal drops. For older children, use a saline nasal spray or saline nasal irrigation.
- Offer cold or frozen drinks or foods. Ice cream, frozen fruit pops, ice or cold beverages might feel good on a sore throat.
- Encourage salt water gargling. For children age 6 years and older, gargling salt water might soothe throat pain.
- Offer hard candy. For children age 5 years and older, sucking on a piece of hard candy might soothe throat pain. Hard candy is probably as effective as medicated lozenges and less likely to have harmful effects. However, hard candy is a choking hazard and shouldn't be given to younger children.
What's the best way to prevent the common cold?
To help your child stay healthy:
- Keep it clean. Teach your child to wash his or her hands thoroughly and often. When soap and water aren't available, provide an alcohol-based hand sanitizer or hand wipes. Keep toys and common household surfaces clean, too.
- Cover up. Teach your child to cough or sneeze into a tissue — and then toss it. If he or she can't reach a tissue in time, show your child how to cough or sneeze into the crook of the arm.
- Steer clear of colds. When possible, help or encourage your child to avoid close contact with anyone who has a cold.
-
Ear infection treatment: Do alternative therapies work?
Alternative ear infection treatments aren't generally recommended for use in children — some have dangerous side effects or may interfere with conventional treatments.
Alternative ear infection treatments abound on the internet and in books and magazines. They include chiropractic adjustments, homeopathy, herbal eardrops and others.
Perhaps you're seeking alternative treatments for your or your child's ear infection because you're concerned about using antibiotics or because your doctor has recommended watchful waiting. You may turn to alternative treatments to ease discomfort.
In most cases, however, researchers haven't studied alternative ear infection treatments adequately using widely accepted scientific methods. For this reason, alternative ear infection treatments aren't generally recommended for use in children.
Some alternative ear infection treatments have been studied with mixed results.
- Homeopathy. A controversial treatment for ear infection, homeopathy involves using highly diluted preparations of natural substances, typically plants and minerals, to treat symptoms of illness.
Study results have been mixed, and it remains unclear whether this treatment is of any benefit. Many such products aren't monitored and are subject to limited regulatory oversight by the Food and Drug Administration. - Chiropractic treatment. This involves manipulating the body so that the skeleton is in alignment. Proponents of chiropractic treatment claim that certain manipulations can prevent or cure ear infections.
No rigorous long-term studies have proved the effectiveness of chiropractic treatment for ear infections. And children may be at increased risk of injury from certain manipulations. - Xylitol. Found in many fruits and used as a natural sweetener in chewing gum, xylitol has been found in some studies to help prevent ear infections but not treat them. To be effective, xylitol needs to be taken in high doses. Abdominal pain and diarrhea are common side effects.
- Probiotics. Certain strains of these "good" bacteria, which occur naturally in the body, may help prevent ear infections in infants and children. Studies have been done on both oral probiotics and nasal sprays with mixed results. Probiotics generally are considered safe and are not known to cause side effects.
Other alternative ear infection treatments that show some possible effect include traditional Chinese medicine, such as acupuncture, and herbal eardrops. But more study is needed to determine the effectiveness and safety of alternative treatments.
Before your child uses an alternative ear infection treatment, be sure to:
- Learn about treatments. Understand your options and what's involved. Find out what benefits their practitioners claim the treatments provide and the potential risks or side effects.
- Find out what the treatment costs. Alternative therapies may not be covered by medical insurance.
- Assess the credentials of anyone who advocates alternative medicine. Gather information from a variety of sources and evaluate the information carefully.
- Tell your doctor. It's important for your doctor to know if you decide to use an alternative therapy. Some treatments — such as herbal supplements — may alter the effect of other therapies or medications. Others may create dangerous drug interactions.
- Homeopathy. A controversial treatment for ear infection, homeopathy involves using highly diluted preparations of natural substances, typically plants and minerals, to treat symptoms of illness.
-
Hand-washing
Hand-washing is an easy way to prevent infection. Understand when to wash your hands, how to properly use hand sanitizer and how to get your children into the habit.
Frequent hand-washing is one of the best ways to avoid getting sick and spreading illness. Find out when and how to wash your hands properly.
When to wash your hands
As you touch people, surfaces and objects throughout the day, you accumulate germs on your hands. You can infect yourself with these germs by touching your eyes, nose or mouth, or spread them to others. Although it's impossible to keep your hands germ-free, washing your hands frequently can help limit the transfer of bacteria, viruses and other microbes.
Always wash your hands before:
- Preparing food or eating
- Treating wounds or caring for a sick person
- Inserting or removing contact lenses
Always wash your hands after:
- Preparing food
- Using the toilet or changing a diaper
- Touching an animal, animal feed or waste
- Blowing your nose, coughing or sneezing
- Treating wounds or caring for a sick person
- Handling garbage
Also, wash your hands when they are visibly dirty.
Skip the antibacterial soap
Antibacterial soaps, such as those containing triclosan, are no more effective at killing germs than is regular soap. Using antibacterial soap might even lead to the development of bacteria that are resistant to the product's antimicrobial agents — making it harder to kill these germs in the future.
In 2016 the Food and Drug Administration issued a rule under which over-the-counter consumer antiseptic wash products containing the majority of the antibacterial active ingredients — including triclosan and triclocarban — can no longer be marketed to consumers. These products include liquid, foam and gel hand soaps, bar soaps, and body washes.
How to wash your hands
It's generally best to wash your hands with soap and water. Follow these steps:
- Wet your hands with running water — either warm or cold.
- Apply liquid, bar or powder soap to a cupped hand.
- Lather well.
- Rub your hands, palm to palm, vigorously for at least 20 seconds. Remember to scrub all surfaces, including the backs of your hands, wrists, between your fingers and under your fingernails.
- Rinse well.
- Dry your hands with a clean towel.
- Use the towel to turn off the faucet.
How to use an alcohol-based hand sanitizer
Alcohol-based hand sanitizers, which don't require water, are an acceptable alternative when soap and water aren't available. If you use a hand sanitizer, make sure the product contains at least 60 percent alcohol. Follow these steps:
- Apply enough of the product to the palm of your hand to wet your hands completely.
- Rub your hands together, covering all surfaces, until your hands are dry.
Kids need clean hands, too
Help children stay healthy by encouraging them to wash their hands frequently. Wash your hands with your child to show him or her how it's done. To prevent rushing, suggest washing hands for as long as it takes to sing the "Happy Birthday" song twice. If your child can't reach the sink on his or her own, keep a step stool handy.
Alcohol-based hand sanitizers are OK for children and adolescents, especially when soap and water aren't available. However, be sure to supervise young children using alcohol-based hand sanitizers. Swallowing alcohol-based sanitizers can cause alcohol poisoning. Store the container safely away after use.
A simple way to stay healthy
Hand-washing offers great rewards in terms of preventing illness. Adopting this habit can play a major role in protecting your health.
Print this "Wash Your Hands" coloring sheet.
-
Infant Massage
Looking for ways to relax and bond with your baby? Understand when and how to give an infant massage.
Infant massage is a way for you to gently nurture and spend time with your baby. Find out about the possible benefits of infant massage and know how to get started.
What are the benefits of infant massage?
Research suggests that infant massage can have various health benefits. For example, infant massage might:
- Encourage interaction between you and your baby
- Help your baby relax and sleep
- Positively affect infant hormones that control stress
- Reduce crying
Although further research is needed, some studies also suggest that infant massage involving moderate pressure might promote growth for premature babies.
When should I massage my baby?
Massaging your baby too soon after a feeding might cause your baby to vomit — so wait at least 45 minutes after a feeding. Also pay close attention to your baby's mood. If your baby has a steady gaze and appears calm and content, he or she might enjoy a massage. If your baby turns his or her head away from you or becomes stiff in your arms, it might not be the best time for a massage.
Once you start massaging your baby, when and how often you massage your baby is up to you. You might give your newborn a daily massage. Your toddler might enjoy a massage at night as a soothing part of his or her bedtime routine.
How do I massage my baby?
Infant massage involves a little preparation and some basic techniques. To get started:
- Create a calm atmosphere. If possible, do the massage in a warm, quiet place — indoors or outdoors. Remove your jewelry. Sit comfortably on the floor or a bed or stand in front of the changing table and position your baby on a blanket or towel in front of you. Place your baby on his or her back so that you can maintain eye contact. As you undress your baby, tell him or her it's massage time.
- Control your touch. When you first start massaging your baby, use a gentle touch. Avoid tickling your baby, however, which might irritate him or her. As your baby grows, use a firmer touch.
- Slowly stroke and knead each part of your baby's body. You might start by placing your baby on his or her stomach and spending one minute each rubbing different areas, including your baby's head, neck, shoulders, upper back, waist, thighs, feet and hands. Next, place your baby on his or her back and spend one minute each extending and flexing your baby's arms and legs, and then both legs at the same time. Finally, with your baby either on his or her back or stomach, repeat the rubbing motions for another five minutes.
- Stay relaxed. Talk to your baby throughout the massage. You might sing or tell a story. Try repeating your baby's name and the word "relax" as you help him or her release tension.
- Watch how your baby responds. If your baby jiggles his or her arms and seems happy, he or she is likely enjoying the massage and you can continue. If your baby turns his or her head away from you or appears restless or unhappy, stop the massage and try again later.
Should I use oil?
It's up to you. Some parents prefer to use oil during infant massage to prevent friction between their hands and the baby's skin, while others find it too messy. If you choose to use oil, select one that's odorless and edible — just in case your baby gets some in his or her mouth. If your baby has sensitive skin or allergies, test the oil first by applying a small amount to a patch of your baby's skin and watching for a reaction.
Is infant massage OK for babies who have health issues?
If your baby has any underlying health issues, talk to your baby's doctor before trying infant massage. The doctor can help you determine if massage is appropriate. You might also ask your baby's doctor if he or she can recommend an infant massage specialist or other qualified expert who can teach you techniques to address your baby's specific needs.
It might take a few tries before you and your baby get the hang of infant massage. Be patient. With a little practice, infant massage can be a healthy way for you and your baby to relax and bond.
-
Sick baby? When to seek medical attention
When a healthy baby gets sick, don't panic. Understand when to call the doctor and when to seek emergency care for your baby.
When you have a baby occasional infections and fevers are inevitable. But even parents who have experience with sick babies can have trouble distinguishing normal fussiness and mild illnesses from serious problems. Here's when to contact the doctor — and when to seek emergency care — for a sick baby.
When to contact your baby's doctor
An occasional illness is usually nothing to worry about in an otherwise healthy baby — but sometimes it's best to contact the doctor. Look for these signs and symptoms:
- Changes in appetite. If your baby refuses several feedings in a row or eats poorly, contact the doctor.
- Changes in behavior. If your baby is hard to awaken or unusually sleepy, tell the doctor right away. Let the doctor know if your baby is extremely floppy, crying more than usual or very hard to console.
- Tender navel or penis. Contact the doctor if your baby's umbilical area or penis suddenly becomes red or starts to ooze or bleed.
- Fever. If your baby is younger than 3 months old, contact the doctor for any fever.
If your baby is 3 to 6 months old and has a temperature up to 102 F (38.9 C) and seems sick or has a temperature higher than 102 F (38.9 C), contact the doctor.
If your baby is 6 to 24 months old and has a temperature higher than 102 F (38.9 C) that lasts longer than one day but shows no other signs or symptoms, contact the doctor. If your baby also has other signs or symptoms — such as a cold, cough or diarrhea — you might contact the doctor sooner based on their severity.
If your baby has a fever that lasts for more than 3 days, contact the doctor. - Diarrhea. Contact the doctor if your baby's stools are especially loose or watery.
- Vomiting. Occasional spitting up, the easy flow of a baby's stomach contents through his or her mouth, is normal. Vomiting occurs when the flow is forceful — shooting out inches rather than dribbling from the mouth. Contact the doctor if your baby vomits forcefully after feedings or your baby hasn't been able to keep liquids down for eight hours.
- Dehydration. Contact the doctor if your baby cries with fewer tears, has significantly fewer wet diapers or has a dry mouth. Also contact the doctor if your baby's soft spot appears sunken.
- Constipation. If your baby has fewer bowel movements than usual for a few days and appears to be struggling or uncomfortable, contact the doctor.
- Colds. Contact the doctor if your baby has a cold that interferes with his or her breathing, has nasal mucus that lasts longer than 10 to 14 days, has ear pain or has a cough that lasts more than one week.
- Rash. Contact the doctor if a rash appears infected or if your baby suddenly develops an unexplained rash — especially if it's accompanied by a fever.
- Eye discharge. If one or both eyes are red or leaking mucus, contact the doctor.
If you think you should contact the doctor, go ahead. After hours, you might be able to use a 24-hour nurse line offered through the doctor's office or your health insurance company.
When to seek emergency care
Seek emergency care for:
- Bleeding that can't be stopped
- Poisoning
- Seizures
- Increasing difficulty breathing
- Any change in consciousness, confusion, a bad headache or vomiting several times after a head injury
- Unconsciousness, acting strangely or becoming more withdrawn and less alert
- Large or deep cuts or burns or smoke inhalation
- Skin or lips that look blue, purple or gray
- Increasing or severe persistent pain
- Major mouth or facial injuries
- Near drowning
Prepare for emergencies in advance by asking your baby's doctor during a checkup what to do and where to go if your baby needs emergency care. Learn basic first aid, including CPR, and keep emergency phone numbers and addresses handy.
Be ready to answer questions
Be prepared to help the medical staff understand what's happening with your baby. Expect questions about:
- Your baby's symptoms. What prompted you to seek medical attention for your baby? What are your specific concerns?
- Your baby's medical history. Does your baby have any known allergies? Are your baby's immunizations current? Does your baby have any chronic conditions? Be prepared to share details about your pregnancy and the baby's birth.
- Changes in your baby's feeding and bowel movements. Have you noticed changes in your baby's eating or drinking patterns, in the number of wet diapers, or in the number, volume or consistency of bowel movements?
- Changes in your baby's temperature. What's your baby's temperature? How did you take it and at what time?
- Home remedies and medications. Have you tried any home remedies or given your baby any over-the-counter or prescription medications? If so, what, how much and when? If you suspect your child ingested poison or medications, bring the bottle with you.
- Possible exposures. Is anyone ill among your household contacts or, if relevant, at your baby's child care center? Have you traveled with your baby recently?
Before you contact your baby's doctor, make sure you're prepared to jot down any instructions. Have your pharmacy's contact information ready, too.
Being prepared will save you and your baby's doctor time during a phone call, office visit or emergency situation.
-
Spitting up: What's normal, what's not
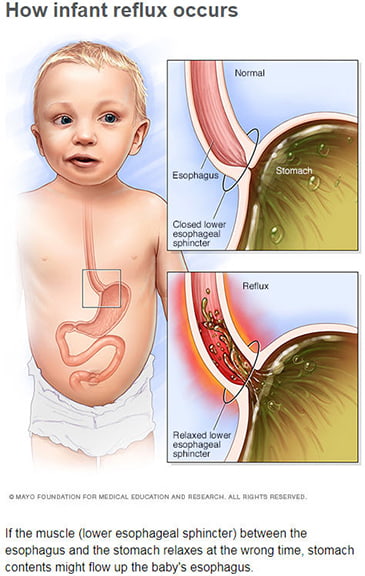 Spitting up is a rite of passage for many babies. Here's what's behind spitting up — and when it might signal a more serious problem.
Spitting up is a rite of passage for many babies. Here's what's behind spitting up — and when it might signal a more serious problem.
You've just fed your baby breast milk or formula only to watch him or her spit up what seems like all of it. Is this normal? Find out the possible causes of spitting up, and what you can do about it.
What causes spitting up?
Spitting up is common in healthy babies. About half of all babies during their first three months experience their stomach contents coming back up into the esophagus, a condition known as gastroesophageal reflux, infant reflux or infant acid reflux.
Normally, a muscle (lower esophageal sphincter) between the esophagus and the stomach keeps stomach contents where they belong. Until this muscle has time to mature, spitting up might be an issue — especially if your baby is relatively full.
What is the difference between spitting up and vomiting?
Spitting up is the easy flow of a baby's stomach contents through his or her mouth, possibly with a burp. Vomiting occurs when the flow is forceful — shooting out inches rather than dribbling from the mouth.
It seems like my baby is spitting up a lot. Can spitting up affect my baby's growth?
Normal spitting up doesn't interfere with a baby's well-being. As long as your baby seems comfortable and is eating well and gaining weight, there's little cause for concern. If your baby is gaining weight, then he or she isn't being harmed by the calories lost through spitting up.
Keep in mind that it's easy to overestimate the amount your baby has spit up based on the size of a spit-up stain.
Will my baby outgrow spitting up?
Most babies stop spitting up by age 12 months.
What can you do to reduce spitting up?
Consider these tips:
- Keep your baby upright. Feed your baby in a more upright position. Follow each feeding with 30 minutes in an upright position. Avoid immediate active play or use of an infant swing.
- Avoid overfeeding. Feeding your baby smaller amounts, more frequently might help.
- Take time to burp your baby. Frequent burps during and after each feeding can keep air from building up in your baby's stomach.
- Put baby to sleep on his or her back. To reduce the risk of sudden infant death syndrome (SIDS), it's important to place your baby to sleep on his or her back. Placing a baby to sleep on his or her tummy to prevent spitting up isn't recommended.
- Experiment with your own diet. If you're breastfeeding, your baby's doctor might suggest that you eliminate dairy products or certain other foods from your diet.
Can spitting up be a sign of a problem?
Certain signs and symptoms might indicate an underlying condition or something more serious than run-of-the-mill spitting up. Contact your baby's doctor if your baby:
- Isn't gaining weight
- Spits up forcefully
- Spits up green or yellow fluid
- Spits up blood or a material that looks like coffee grounds
- Refuses feedings repeatedly
- Has blood in his or her stool
- Has difficulty breathing or other signs of illness
- Begins spitting up at age 6 months or older
Treatment depends on what's causing the problem. Special feeding techniques might be helpful. In other cases, the doctor might prescribe medication to treat reflux.
-
Teething
Is your teething baby keeping you up at night? Understand how to soothe sore gums and care for your baby's new teeth.
Drooling, crankiness and tears can make teething an ordeal for babies and parents alike. Here's information to help ease the pain — for both of you.
What's typical?
Although timing varies widely, babies often begin teething by about age 6 months. The two bottom front teeth (lower central incisors) are usually the first to appear, followed by the two top front teeth (upper central incisors).
Classic signs and symptoms of teething include:
- Drooling
- Chewing on objects
- Irritability or crankiness
- Sore or tender gums
- Low-grade rectal fever of 99 F (37.2 C)
Many parents suspect that teething causes higher fever and diarrhea, but researchers say they aren't indications of teething. If your baby has a rectal temperature of 100.4 F (38 C) or diarrhea, talk to your doctor.
What's the best way to soothe sore gums?
If your teething baby seems uncomfortable, consider these simple tips:
- Rub your baby's gums. Use a clean finger or moistened gauze pad to rub your baby's gums. The pressure can ease your baby's discomfort.
- Keep it cool. A cold washcloth, spoon or chilled teething ring can be soothing on a baby's gums. Don't give your baby a frozen teething ring, however.
- Try hard foods. If your baby is eating solid foods, you might offer something edible for gnawing — such as a peeled and chilled cucumber or carrot. Keep a close eye on your baby, however. Any pieces that break off might pose a choking hazard.
- Dry the drool. Excessive drooling is part of the teething process. Having a teething ring, fingers or other objects in the mouth produces saliva. To prevent skin irritation, keep a clean cloth handy to dry your baby's chin. Consider applying a moisturizer such as a water-based cream or lotion.
- Try an over-the-counter remedy. If your baby is especially cranky, acetaminophen (Tylenol, others) or ibuprofen (Advil, Children's Motrin, others) might help.
Avoid homeopathic teething tablets and teething medications that contain the pain reliever benzocaine or lidocaine. They can be harmful — even fatal — to your baby.
Do I need to call the doctor?
Teething can usually be handled at home. Contact the doctor if your baby develops a fever, seems particularly uncomfortable, or has other signs or symptoms of illness that could be unrelated to the teething.
How do I care for my baby's new teeth?
Ideally, you've been running a clean, damp washcloth or a soft infant toothbrush over your baby's gums every day. If not, now's a great time to start. The cleansing can keep bacteria from building up in your baby's mouth.
When your baby's first teeth appear, use a small, soft-bristled toothbrush. Until your child learns to spit — at about age 3 — use a smear of fluoride toothpaste no bigger than the size of a grain of rice. Then switch to a pea-sized dollop as they approach 2 to 3 years of age.
It's also time to think about regular dental checkups. The American Dental Association and the American Academy of Pediatric Dentistry recommend scheduling a child's first dental visit after the first tooth erupts and no later than his or her first birthday.
Your baby's teeth and gums will also be examined at well-baby checkups. Remember, regular childhood dental care helps set the stage for a lifetime of healthy teeth and gums.
-
Thermometer Basics
Thermometer choices got you baffled? Understand the different thermometer options — and when to seek medical help for a fever.
If your child feels warm or seems under the weather, it's probably time to take his or her temperature. Sounds simple enough — but if you're new to it, you might have questions. Which type of thermometer is best? Are thermometer guidelines different for babies and older children? Here's what you need to know to take your child's temperature.
Thermometer options
A glass mercury thermometer was once a staple in most medicine cabinets. Today, mercury thermometers are no longer recommended because they can break and allow mercury to vaporize and be inhaled. When choosing a thermometer, consider these options:
- Digital thermometers. These thermometers use electronic heat sensors to record body temperature. They can be used in the rectum (rectal), mouth (oral) or armpit (axillary). Armpit temperatures are typically the least accurate of the three.
- Digital ear thermometers (tympanic membrane). These thermometers use an infrared ray to measure the temperature inside the ear canal. Keep in mind that earwax or a small, curved ear canal can interfere with the accuracy of an ear thermometer temperature.
- Temporal artery thermometers. These thermometers use an infrared scanner to measure the temperature of the temporal artery in the forehead. This type of thermometer can be used even while a child is asleep.
Digital pacifier thermometers and fever strips are not recommended.
Safety tips
Carefully read the instructions that come with the thermometer. Before and after each use, clean the tip of the thermometer with rubbing alcohol or soap and lukewarm water and then rinse with cool water. If you plan to use a digital thermometer to take a rectal temperature, get another digital thermometer for oral use. Label each thermometer, and don't use the same thermometer in both places.
For safety — and to make sure the thermometer stays in place — never leave your child unattended while you're taking his or her temperature.
Age guidelines
The best type of thermometer — or the best place to insert the thermometer, in some cases — depends on your child's age.
- Birth to 3 months. Use a regular digital thermometer to take a rectal temperature. New research suggests that a temporal artery thermometer might also provide accurate readings in newborns.
- 3 months to 4 years. In this age range you can use a digital thermometer to take a rectal or an armpit temperature or you can use a temporal artery thermometer. However, wait until your baby is at least 6 months old to use a digital ear thermometer. If you use another type of thermometer to take a young child's temperature and you're in doubt about the results, take a rectal temperature.
- 4 years and older. By age 4, most kids can hold a digital thermometer under the tongue for the short time it takes to get an oral temperature reading. You can also use a digital thermometer to take an armpit temperature, or use a temporal artery thermometer or a digital ear thermometer.
How it's done
- Rectal temperature. Turn on the digital thermometer and lubricate the tip of the thermometer with petroleum jelly. Lay your baby or child on his or her back, lift his or her thighs, and insert the lubricated thermometer 1/2 to 1 inch (1.3 to 2.5 centimeters) into the rectum. Never try to force the thermometer past any resistance. Hold the thermometer in place until the thermometer signals that it's done. Remove the thermometer and read the number.
- Oral temperature. Turn on the digital thermometer. Place the tip of the thermometer under your child's tongue toward the back of the mouth and ask your child to keep his or her lips closed. Remove the thermometer when it signals that it's done and read the number. If your child has been eating or drinking, wait 15 minutes to take his or her temperature by mouth.
- Armpit temperature. Turn on the digital thermometer. When you place the thermometer under your child's armpit, make sure it touches skin — not clothing. Hold the thermometer tightly in place until the thermometer signals that it's done. Remove the thermometer and read the number.
- Ear temperature. Turn on the thermometer. Gently place the thermometer in your child's ear. Follow the directions that come with the thermometer to ensure you insert the thermometer the proper distance into the ear canal. Hold the thermometer tightly in place until the thermometer signals that it's done. Remove the thermometer and read the number.
- Temporal artery temperature. Turn on the thermometer. Gently sweep the thermometer across your child's forehead. Remove the thermometer and read the number.
When reporting a temperature to your child's doctor, give the reading and explain how the temperature was taken.
When to see a doctor
A fever is a common sign of illness, but that's not necessarily a bad thing. In fact, fevers seem to play a key role in fighting infections. If your child is older than age 6 months and is drinking plenty of fluids, sleeping well and continuing to play, there's usually no need to treat the fever.
If you want to give your child medication to treat a fever, stick to acetaminophen (Tylenol, others) until age 6 months. However, for children younger than age 3 months, don't give acetaminophen until your baby has been seen by a doctor. Never give more acetaminophen than recommended on the label for your child. Be aware that some combination over-the-counter medications might contain acetaminophen as an ingredient.
If your child is age 6 months or older, ibuprofen (Advil, Children's Motrin, others) is OK, too. Read the label carefully for proper dosage. Don't use aspirin to treat a fever in anyone age 18 years or younger.
Your child has a fever if he or she:
- Has a rectal, ear or temporal artery temperature of 100.4 F (38 C) or higher
- Has an oral temperature of 100 F (37.8 C) or higher
- Has an armpit temperature of 99 F (37.2 C) or higher
Keep in mind that an armpit temperature might not be accurate. If you're in doubt about an armpit temperature reading, use another method to confirm the results.
In general, contact your child's doctor if:
- Your child is younger than age 3 months and has a rectal temperature of 100.4 F (38 C) or higher.
- Your child is age 3 to 6 months and has a temperature up to 102 F (38.9 C) and seems unusually irritable, lethargic or uncomfortable, or has a temperature higher than 102 F (38.9 C).
- Your child is age 6 to 24 months and has a temperature higher than 102 F (38.9 C) that lasts longer than one day but shows no other signs. If your child has other signs, such as a cold, cough or diarrhea, you might call your child's doctor sooner based on their severity.
-
Thermometers: Understand the options
Thermometers come in a variety of styles. Understand the different types of thermometers and how to pick the right thermometer for you.
Choosing the thermometer that's best for your family can be confusing. Here's what you need to know about the most common thermometers.
Digital thermometers
Regular digital thermometers use electronic heat sensors to record body temperature. These thermometers can be used in the rectum, mouth or armpit.
Armpit temperatures are usually the least accurate. Rectal temperatures provide the best readings for infants, especially those 3 months or younger, as well as children up to age 3. For older children and adults, oral readings are usually accurate — as long as the mouth is closed while the thermometer is in place.
If you plan to use a digital thermometer to take both oral and rectal temperatures, you'll need to get two digital thermometers and label one for oral use and one for rectal use. Don't use the same thermometer in both places.
The pros:
- Most digital thermometers can record temperatures from the mouth, armpit or rectum — often in a minute or less.
- A digital thermometer is appropriate for newborns, infants, children and adults.
The cons:
- Parents may worry about causing discomfort when taking a child's temperature rectally.
- You need to wait 15 minutes after eating or drinking to take an oral temperature. Otherwise, the temperature of your food or drink might affect the thermometer reading.
- It can be difficult for children — or anyone who breathes through the mouth — to keep their mouths closed long enough to get an accurate oral reading.
Digital ear thermometers
Digital ear thermometers, also called tympanic thermometers, use an infrared ray to measure the temperature inside the ear canal.
The pros:
- When positioned properly, digital ear thermometers are quick and generally comfortable for children and adults.
- Digital ear thermometers are appropriate for infants older than age 6 months, older children and adults.
The cons:
- Digital ear thermometers aren't recommended for newborns.
- Earwax or a small, curved ear canal can interfere with the accuracy of a temperature taken with a digital ear thermometer.
Digital pacifier thermometers
If your child uses a pacifier, you might want to try a digital pacifier thermometer. Your child simply sucks on the pacifier until the peak temperature is recorded.
The pro:
- Your child may not even realize you're taking his or her temperature.
The cons:
- Digital pacifier thermometers aren't recommended for newborns.
- For the most accurate reading, your child must hold the pacifier still in his or her mouth for about three to five minutes — which is difficult for many young children.
- Recent research doesn't support the accuracy of temperature readings from pacifier thermometers.
Temporal artery thermometers
Temporal artery thermometers — often sold as forehead thermometers — use an infrared scanner to measure the temperature of the temporal artery in the forehead.
The pros:
- Temporal artery thermometers can record a person's temperature quickly and are easily tolerated.
- Temporal artery thermometers are appropriate for infants older than age 3 months and for older children. New research suggests that a temporal artery thermometer also might provide accurate readings for a newborn.
- Additional research suggests that temporal artery thermometers are the most accurate alternative to rectal digital thermometers for taking a child's temperature.
The con:
- A temporal artery thermometer may be more expensive than other types of thermometers.
Mercury thermometers
Once a staple in most medicine cabinets, mercury thermometers use mercury encased in glass to measure body temperature. Mercury thermometers are no longer recommended because they can break and allow mercury — which is toxic — to escape.
If you have a mercury thermometer, don't throw it in the trash. Contact your local trash collection program to see if there's a hazardous waste collection site in your area.
-
Umbilical cord care
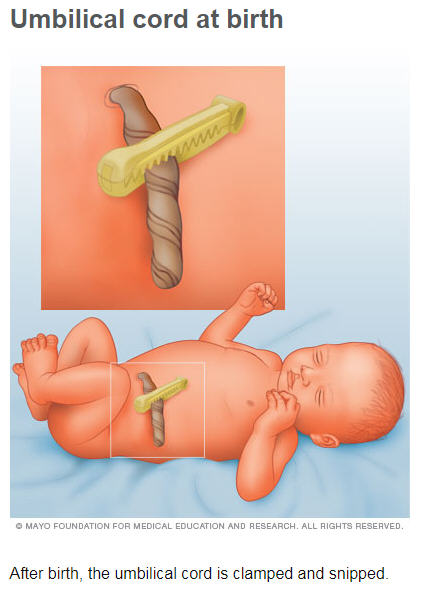 A newborn's umbilical cord stump typically falls off within about two weeks after birth. In the meantime, treat your baby's umbilical cord stump gently.
A newborn's umbilical cord stump typically falls off within about two weeks after birth. In the meantime, treat your baby's umbilical cord stump gently.
Wonder how to care for your newborn's umbilical cord stump? Follow these tips to promote healing.
Why your baby has an umbilical cord stump
Multimedia Image of umbilical cord at birth Umbilical cord at birth During pregnancy, the umbilical cord supplies nutrients and oxygen to your developing baby. After birth, the umbilical cord is no longer needed — so it's clamped and snipped. This leaves behind a short stump.
Taking care of the stump
Your baby's umbilical cord stump will change from bluish white to black as it dries out and eventually falls off — usually within three weeks after birth. In the meantime, treat the area gently:
- Keep the stump clean. Parents were once instructed to swab the stump with rubbing alcohol after every diaper change. Researchers now say the stump might heal faster if left alone. If the stump becomes dirty or sticky, clean it with plain water — then dry it by holding a clean, absorbent cloth around the stump or fanning it with a piece of paper.
- Keep the stump dry. Expose the stump to air to help dry out the base. Keep the front of your baby's diaper folded down to avoid covering the stump. In warm weather, dress your baby in a diaper and T-shirt to improve air circulation.
- Stick with sponge baths. Sponge baths might be most practical during the healing process. When the stump falls off, you can bathe your baby in a baby tub or sink.
- Let the stump fall off on its own. Resist the temptation to pull off the stump yourself.
Signs of infection
During the healing process, it's normal to see a little blood near the stump. Much like a scab, when the cord stump falls off, a little bleeding might occur. However, contact your baby's doctor if the umbilical area ooze pus or the surrounding skin becomes red and swollen. If your baby has an umbilical cord infection, prompt treatment is needed to stop the infection from spreading
.
-
Well-baby Exam: What to Expect
Well-baby exam: What to expect during routine checkups A well-baby exam involves measurements, vaccines and an evaluation of your baby's development. Know the basics of a well-baby exam and how to prepare.
Well-baby exams, or regular checkups, are an important way to monitor your baby's growth and development. These exams also provide an opportunity to develop a relationship with your baby's doctor.
Your baby's doctor will likely recommend the first well-baby exam within three to five days after birth, or shortly after you're discharged from the hospital. Additional well-baby exams will be needed every few weeks and, later, months for the first year. In some cases, the baby's doctor might want more frequent checkups. Here's what's on the agenda during these exams.
Your baby's measurements
A well-baby exam usually begins with measurements. You'll need to undress your baby so he or she can be accurately weighed on an infant scale. Length will be measured by placing your baby on a flat surface and stretching his or her legs out. A special tape will be used to measure his or her head circumference.
The measurements will be plotted on a growth chart to determine your baby's growth curve. This will help determine if your baby is growing normally and show how his or her growth compares to other children of the same age.
Head-to-toe physical exam
Expect a thorough physical exam during the checkup. Mention any concerns you have or areas you want the doctor to check out. Here are the basics:
- Head. The doctor will check the soft spots (fontanels) on your baby's head. These gaps between the skull bones are safe to touch and give your baby's brain room to grow. The doctor will check the shape of your baby's head as well.
- Ears. The doctor will check for fluid or infection in your baby's ears with an instrument called an otoscope. He or she might observe your baby's response to various sounds, including your voice.
- Eyes. He or she might also look inside your baby's eyes with an instrument called an ophthalmoscope. As your baby gets older, the doctor might use a bright object or flashlight to catch your baby's attention and then track your baby's eye movements.
- Mouth. A look inside your baby's mouth might reveal signs of oral thrush, a common — and easily treated — yeast infection. As your baby gets older, the doctor might ask whether you've noticed more drooling or chewing than usual. These are often the first signs of teething.
- Skin. Various skin conditions might be identified during the exam, including birthmarks and rashes.
- Heart and lungs. The doctor will listen to your baby's heart and lungs with a stethoscope to detect any abnormal heart sounds or rhythms or breathing difficulties. Heart murmurs are often innocent, yet sometimes consultation with a specialist is recommended.
- Abdomen. By gently pressing your baby's abdomen, the doctor can detect tenderness, enlarged organs or an umbilical hernia, which occurs when a bit of intestine or fatty tissue near the navel breaks through the muscular wall of the abdomen.
- Hips and legs. The doctor might move your baby's legs to check for dislocation or other problems with the hip joints.
- Genitalia. The doctor will likely inspect your baby's genitalia for tenderness, lumps or other signs of infection. For girls, the doctor might ask about vaginal discharge. For boys, the doctor will make sure both testes have descended into the scrotum and, in the case of circumcision, whether the penis is healing properly.
Unless your baby has special needs or concerns, lab tests aren't needed at most well-baby exams.
Your baby's development Your baby's motor skills and development are important, too. Depending on your baby's age, be prepared to answer questions like these:
- How well does your baby control his or her head?
- Does your baby imitate your facial expressions and sounds?
- Does your baby reach for objects or put them into his or her mouth?
- Does your baby attempt to roll over?
- Can your baby sit with support?
- Does your baby pull up into a standing position?
- Does your baby use individual fingers to pick up small objects?
Your baby's vaccines
Your baby will need various vaccines at well-baby visits. During each injection, the doctor will instruct you on how to hold your baby and help keep him or her still. Afterward, hold your baby, talk, sing, breast-feed or offer your baby a bottle to help soothe him or her.
Time to talk
During the appointment, your baby's doctor will likely ask how things are going. Be ready to describe a typical day with your baby. For example:
- How many hours does your baby sleep during the day? At night?
- How often do you feed your baby? If you're breastfeeding, are you having any trouble?
- How many diapers does your baby wet and soil in a day?
- How active is your baby?
- Are you including tummy time in your baby's activities?
- How is your baby's temperament?
In addition, your baby's doctor might ask questions about your family's home life and medical history. The doctor might also discuss safety issues, such as placing your baby to sleep on his or her back and using a rear-facing infant car seat. Although breast milk or formula will be the main part of your baby's diet throughout the first year, you'll also talk about when to introduce solid foods.
Undoubtedly, you'll have questions, too. Ask away! Consider writing down your questions beforehand so you don't forget them in the moment. If you and your partner can't both attend the visit, ask a relative or friend to come with you to help care for your baby while you talk to the doctor.
Also remember your own health. If you're feeling depressed, stressed out or run-down, describe what's happening. Your baby's doctor is there to help you, too.
Heading home
Make sure you know when to schedule your baby's next appointment — and how to reach the doctor in the meantime. Ask if the doctor's office or clinic offers a 24-hour nurse information service. Knowing help is available when you need it can offer peace of mind.
Nutrition and Fitness
-
Babies and Solid Food
Solid foods are a big step for a baby. Find out when and how to make the transition from breast milk or formula to solid foods.
Giving your baby his or her first taste of solid food is a major milestone. Here's what you need to know before your baby takes that first bite.
Is your baby ready for solid foods?
Breast milk or formula is the only food your newborn needs, and the American Academy of Pediatrics recommends exclusive breastfeeding for the first six months after birth.
But by ages 4 months to 6 months, most babies are ready to begin eating solid foods as a complement to breastfeeding or formula-feeding. It's during this time that babies typically stop using their tongues to push food out of their mouths and begin to develop the coordination to move solid food from the front of the mouth to the back for swallowing.
In addition to age, look for other signs that your baby is ready for solid foods. For example:
- Can your baby hold his or her head in a steady, upright position?
- Can your baby sit with support?
- Is your baby mouthing his or her hands or toys?
- Is your baby interested in what you're eating?
If you answer yes to these questions and your baby's doctor agrees, you can begin supplementing your baby's liquid diet.
What to serve when
Continue feeding your baby breast milk or formula — up to 32 ounces a day. Then:
- Start simple. Offer single-ingredient foods that contain no sugar or salt, and wait three to five days between each new food. This way if your baby has a reaction — such as diarrhea, rash or vomiting — you'll know the cause. After introducing single-ingredient foods, you can offer them in combination.
- Important nutrients. Iron and zinc are important nutrients in the second half of your baby's first year. These nutrients are found in pureed meats and single-grain, iron-fortified cereal. Beans, lentils or other culturally acceptable foods might also be appropriate.
- Baby cereal basics. Mix 1 tablespoon of a single-grain, iron-fortified baby cereal with 4 tablespoons (60 milliliters) of breast milk or formula. Don't serve it from a bottle. Instead, help your baby sit upright and offer the cereal with a small spoon once or twice a day. Serve one or two teaspoons after a bottle- or breastfeeding. Once your baby gets the hang of swallowing runny cereal, mix it with less liquid and gradually increase the amount you offer. Offer a variety of single-grain cereals such as rice, oatmeal or barley. Avoid offering only rice cereal due to possible exposure to arsenic.
- Add vegetables and fruits. Continue gradually introducing single-ingredient foods that contain no sugar or salt. Start with pureed vegetables and then offer fruits. Wait three to five days between each new food.
- Offer finely chopped finger foods. By ages 8 months to 10 months, most babies can handle small portions of finely chopped finger foods, such as soft fruits, vegetables, pasta, cheese, well-cooked meat, baby crackers and dry cereal. As your baby approaches age 1, offer your baby three meals a day — as well as snacks — with mashed or chopped versions of whatever you're eating.
What if my baby refuses his or her first feeding?
This is not unusual. Babies often reject their first servings of pureed foods because the taste and texture is new. If your baby refuses the feeding, don't force it. Try again in a week. If the problem continues, talk to your baby's doctor to make sure the resistance isn't a sign of a problem.
What about food allergies?
To help prevent food allergies, parents were once told to avoid feeding young children highly allergenic foods such as eggs, fish, peanuts and tree nuts. Today, however, there's no convincing evidence that avoiding these foods during early childhood will help prevent food allergies. New research also suggests that desensitizing at-risk children to peanuts between ages 4 and 11 months may be effective at preventing peanut allergies.
In a recent study, high-risk children — such as those with atopic dermatitis or egg allergy or both — were selected to either eat or avoid peanut products from 4 to 11 months of age until 5 years of age. Researchers found that high-risk children who regularly consumed peanut protein, such as peanut butter or peanut-flavored snacks, were 70 to 86 percent less likely to develop a peanut allergy. These findings might impact food allergy guidelines in the future.
Still, especially if any close relatives have a food allergy, give your child his or her first taste of a highly allergenic food at home — rather than at a restaurant — with an oral antihistamine available.
Is juice OK?
Juice isn't a necessary part of a baby's diet, and it's not as valuable as whole fruit. Too much juice might contribute to weight problems and diarrhea, as well as thwart your baby's appetite for more-nutritious solid foods. Sipping juice throughout the day or while falling asleep can lead to tooth decay.
If you offer juice, wait until your baby is at least 6 months or older. Make sure the juice is 100 percent fruit juice. Limit the amount your baby drinks to 4 to 6 ounces (118 to 177 milliliters) a day — about one food serving of fruit — and serve it in a cup. Juices containing vitamin C might improve your baby's absorption of iron.
Know what's off-limits
Certain foods are not appropriate for babies. Consider these guidelines:
- Don't offer cow's milk or honey before age 1. Cow's milk doesn't meet an infant's nutritional needs — it isn't a good source of iron — and can increase the risk of iron deficiency. Honey might contain spores that can cause a serious illness known as infant botulism.
- Don't offer foods that can cause your baby to choke. As your baby progresses in eating solid foods, don't offer hot dogs, chunks of meat or cheese, grapes, raw vegetables, or fruit chunks, unless they're cut up into small pieces. Also, don't offer hard foods, such as seeds, nuts, popcorn and hard candy that can't be changed to make them safe options. Other high-risk foods include peanut butter and marshmallows.
Preparing baby food at home
Another reason to avoid giving your baby solid food before age 4 months is the risk associated with certain home-prepared foods. A baby younger than age 4 months should not be given home-prepared spinach, beets, carrots, green beans or squash. These foods might contain enough nitrates to cause the blood disorder methemoglobinemia.
Make meals manageable
When feeding your baby, give him or her your full attention. Talk to your baby and help him or her through the process. In addition, to make mealtime enjoyable:
- Stay seated. As soon as your baby can sit easily without support, use a highchair with a broad, stable base. Buckle the safety straps.
- Encourage exploration. Your baby is likely to play with his or her food. Although it's messy, hands-on fun helps fuel development. Just make sure that finger foods are soft, easy to swallow and broken down into small pieces.
- Introduce utensils. Offer your baby a spoon to hold while you feed him or her with another spoon. As your baby's dexterity improves, encourage your baby to use a spoon.
- Offer a cup. Feeding your baby breast milk or formula from a cup at mealtime can help pave the way for weaning from a bottle. Around age 9 months, your baby might be able to drink from a cup on his or her own.
- Dish individual servings. If you feed your baby directly from a jar or container, saliva on the spoon can quickly spoil leftovers. Instead, place servings in a dish. Opened jars of baby food can be safely refrigerated for two to three days.
- Avoid power struggles. If your baby turns away from a new food, don't push. Simply try again another time. Repeated exposure can help ensure variety in your baby's diet.
- Know when to call it quits. When your baby has had enough to eat, he or she might cry or turn away. Don't force extra bites. As long as your baby's growth is on target, he or she is likely getting enough to eat. Also, don't try to get your baby to eat as much as possible at bedtime to get him or her to sleep through the night. There's no evidence that this works.
Enjoy your baby's sloppy tray, gooey hands and sticky face. You're building the foundation for a lifetime of healthy eating.
-
Fitness ideas for the entire family
Exercising as a family benefits everyone. As you work toward your own fitness goals, you set an excellent example for your children of committing to their own physical activity. So get creative and find ways to be active together, from playing tag with your toddler to rock climbing with your teen.
If you're a parent, getting into the habit of exercising as a family will benefit both you and your children. As you work toward your own fitness goals, you'll set an excellent example for your children of committing to their own physical activity.
Want to make exercise and family time a top priority? You can do both — just combine the two to maximize your time. In fact, merging the two is a necessity for many busy parents. Here are some ideas for incorporating physical activity at every stage of your kids' lives.
Toddlers to preschoolers
Acknowledge and take advantage of the fact that your child is now on the move.
- Explore a playground where you can run with your child. Remember, you can play on the playground equipment, too! If your child wants to swing, use that time to get in a few squats and lunges. If the playground has a jungle gym, try some pullups, chin-ups or pushups.
- Play active games such as soccer, football or tag.
- Make up your own family game that involves a unique combination of jumping, sprinting, lunging, squatting and crawling. You'll get your heart rate up and incorporate some body weight resistance exercise.
- Create a scavenger hunt and race your child to finish the tasks.
School-age kids
Explore the world with your child. Get involved in the things they enjoy doing.
- Take a walk or hike in nature. Not only will you all get great exercise, but without any electronics around, your child might enjoy talking to you.
- Invest in bikes and explore your city or town for new routes. Ride your bike or walk to lunch or dinner with the family.
- Dance. Just do it — let loose with your kids, have fun and get some great aerobic activity. Put on music your kids like (or some old-school rock they will laugh at) and get moving.
- Swim. When you go to the pool with your children, get in. Running in the shallow end and swimming in a pool are great ways to combine aerobic activity with family fun.
- Get involved in a sport that your kids can enjoy, such as tennis, basketball or soccer.
- Plan vacations in destinations that encourage outdoor activities. Find a vacation spot where you can ski, hike, surf or go rock climbing.
Wherever you go, look for opportunities to add more physical activity to your family life. You'll enjoy time with each other and set your children up with healthy habits for the future.
Experiments
Try these suggestions to create family fitness fun.
- Sit down with your kids and make a family activity plan.
- Head outdoors for some exercise two times this week.
- Try a family yoga session.
-
Getting Kids in the Kitchen
Kids often want to just stick to eating their same-old favorite foods. But, often those aren’t the healthiest for them, and some variety would do them good. Learn how getting kids in the kitchen can also get them to try new things by watching the video below.
-
Infant Formula Basics
Here's what you need to know to choose the best formula for your baby.
If you're planning to feed your baby infant formula, you might have questions. Is one brand of infant formula better than another? Are generic brands OK? Is soy-based formula better than cow's milk formula? Here's what you need to know about infant formula.
What are the main types of infant formula?
Commercial infant formulas are regulated by the Food and Drug Administration (FDA). Three major types are available:
- Cow milk protein-based formulas. Most infant formula is made with cow's milk that's been altered to resemble breast milk. This gives the formula the right balance of nutrients — and makes the formula easier to digest. Most babies do well on cow's milk formula. Some babies, however — such as those allergic to the proteins in cow's milk — need other types of infant formula.
- Soy-based formulas. Soy-based formulas can be useful if you want to exclude animal proteins from your child's diet. Soy-based infant formulas might also be an option for babies who are intolerant or allergic to cow's milk formula or to lactose, a carbohydrate naturally found in cow's milk. However, babies who are allergic to cow's milk might also be allergic to soy milk.
- Protein hydrolysate formulas. These types of formulas contain protein that's been broken down (hydrolyzed) — partially or extensively — into smaller sizes than are those in cow's milk and soy-based formulas. Protein hydrolysate formulas are meant for babies who don't tolerate cow's milk or soy-based formulas. Extensively hydrolyzed formulas are an option for babies who have a protein allergy.
In addition, specialized formulas are available for premature infants and babies who have specific medical conditions.
What infant formula preparations are available?
Infant formulas come in three forms. The best choice depends on your budget and desire for convenience:
- Powdered formula. Powdered formula is the least expensive. Each scoop of powdered formula must be mixed with water.
- Concentrated liquid formula. This type of formula also must be mixed with water.
- Ready-to-use formula. Ready-to-use formula is the most convenient type of infant formula. It doesn't need to be mixed with water. It's also the most expensive option.
Be sure to wash your hands before handling formula and carefully follow any mixing and storage instructions.
What's the difference between generic and brand-name infant formula?
All infant formulas sold in the United States must meet the nutrient standards set by the FDA. Although manufacturers might vary in their formula recipes, the FDA requires that all formulas contain the minimum recommended amount of nutrients that infants need.
Is it important to buy iron-fortified infant formula?
Yes. Your baby needs iron to grow and develop, especially during infancy. If you're not breastfeeding, using iron-fortified formula is the easiest way to provide this essential nutrient.
What about enhanced infant formula?
Some infant formulas are enhanced with docosahexaenoic acid (DHA) and arachidonic acid (ARA). These are omega-3 fatty acids found in breast milk and certain foods, such as fish and eggs. Some studies suggest that including DHA and ARA in infant formula can help infant eyesight and brain development, but other research has shown no benefit.
In addition, many infant formulas include pre- and probiotics — substances that promote the presence of healthy bacteria in the intestines — in an effort to mimic the immune benefits of breast milk. Early studies are encouraging, but long-term benefits of these substances are unknown.
If you're unsure about enhanced infant formula, ask your child's doctor for guidance.
How important is the expiration date on infant formula?
Don't buy or use outdated infant formula. If the expiration date has passed, you can't be sure of the formula's quality.
How long should a child drink infant formula?
Infant formula is generally recommended until age 1, followed by whole milk until age 2 — but talk to your child's doctor for specific guidance. Reduced-fat or skim milk generally isn't appropriate before age 2 because it doesn't have enough calories or fat to promote early brain development.
-
Infant Formula Preparation
Are you measuring your baby's infant formula correctly? Storing it properly? Keeping the utensils clean? To make sure, follow these seven steps.
You've chosen your baby's infant formula with care — but are you preparing it properly? Follow these steps to ensure proper nutrition and avoid food-related illness.
1. Check the expiration date
Look for an expiration or "use by" date on the formula container. If the expiration date has passed, you can't be sure of the formula's quality. Don't buy or use outdated infant formula.
2. Wash your hands
Before preparing formula, wash your hands thoroughly with soap and water. Dry your hands well.
3. Prepare your bottle
Sterilize bottles, nipples, caps and rings before using them for the first time. You can boil the bottle and accessories in water for five minutes, use a microwave steam sterilizer bag or use a stand-alone electric steam sterilizer.
After the first use, there's no need to sterilize your bottle and accessories. Wash these items with soap and water and allow them to air-dry. Bottle and nipple brushes can help you clean nooks and crannies. You can also use a dishwasher.
4. Add water to liquid-concentrate or powdered formula
If you're using liquid-concentrate or powdered formula, you'll need to add water. Follow the manufacturer's instructions for how much water to use.
You can use any type of clean water — tap or bottled — to prepare liquid-concentrate or powdered formula. If you use well water or you're concerned about the purity of your water supply, talk to your baby's doctor or the water department. Well water needs regular testing. To kill bacteria that might be present in municipal water, use tap water that has been boiled for one minute and cooled quickly to body temperature, 98.6 F (37 C). Then, mix the water with formula.
It's also important to consider the amount of fluoride in the water you use to prepare your baby's liquid-concentrate or powdered formula. Exposure to fluoride during infancy helps prevent tooth decay during infancy. However, regularly mixing powdered or liquid concentrate formula with fluoridated water might increase your child's risk of developing faint white lines or streaks on the teeth (fluorosis) if these kinds of formula are your child's main source of food.
If you're concerned about fluorosis, consider ways to minimize your baby's exposure to fluoride. For example, you might use ready-to-feed formula, which contains little fluoride, or alternate between using fluoridated tap water and low-fluoride bottled water — such as purified, demineralized, deionized or distilled bottled water — to prepare concentrated formula. However, if you feed your baby only ready-to-feed formula or concentrated formula mixed with low-fluoride water, your baby's doctor might recommend fluoride supplements beginning at 6 months.
5. Measure the formula
For ready-to-use formula:
- Shake the formula well.
- Pour enough formula for one feeding into a clean bottle.
- Use only formula — don't add water or any other liquid.
- Attach the nipple and cap.
For liquid-concentrate formula:
- Shake the concentrated liquid before mixing it with water.
- Pour the amount of formula for one serving into the bottle, which already contains the appropriate amount of water.
- Attach the nipple and cap and shake well.
For powdered formula:
- Determine the amount of formula you want to prepare, following instructions on the package.
- Use a measuring cup to measure the amount of water needed and add the water to the bottle.
- Use the scoop that came with the formula container. Fill the scoop with powdered formula. Add the number of scoops needed.
- Pour the scoop or scoops into the bottle.
- Attach the nipple and cap and shake well.
6. Warm the formula, if needed
It's fine to give your baby room temperature or even cold formula. If your baby prefers warm formula place a filled bottle in a bowl of warm water and let it stand for a few minutes — or warm the bottle under running water. The formula should feel lukewarm — not hot.
Don't warm bottles in the microwave. The formula might heat unevenly, creating hot spots that could burn your baby's mouth.
Discard remaining formula at the end of each feeding if it has been more than an hour from the start of a feeding. Resist the urge to refrigerate a bottle once you have fed your baby from it, since bacteria from your baby's mouth can still multiply in the refrigerator.
7. Store formula safely
If you're using ready-to-use formula, cover and refrigerate any unused formula from a freshly opened container. Discard any leftover formula that's been in the refrigerator more than 48 hours.
If you prepare and fill several bottles of liquid-concentrate or powdered formula at once:
- Label each bottle with the date that the formula was prepared.
- Refrigerate the extra bottles until you need them.
- Discard any prepared formula that's been in the refrigerator more than 24 hours.
If you're unsure whether a particular container or bottle of formula is safe, throw it out. Don't freeze formula, which can cause the product's components to break down.
-
Iron deficiency
Iron deficiency in children can affect development and lead to anemia. Find out how much iron your child needs, the best sources of iron and more.
Is your child getting enough iron in his or her diet? Find out what causes iron deficiency in children, how to recognize it and how to prevent it.
Why is iron important for children?
Iron is a nutrient that's essential to your child's growth and development. Iron helps move oxygen from the lungs to the rest of the body and helps muscles store and use oxygen. If your child's diet lacks iron, he or she might develop a condition called iron deficiency.
Iron deficiency in children can occur at many levels, from depleted iron stores to anemia — a condition in which blood lacks adequate healthy red blood cells. Untreated iron deficiency can affect a child's growth and development.
How much iron do children need?
Babies are born with iron stored in their bodies, but a steady amount of additional iron is needed to fuel a child's rapid growth and development. Here's a guide to iron needs at different ages:
- 7-12 months: 11 mg
- 1-3 years: 7 mg
- 4-8 years: 10 mg
- 9-13 years: 8 mg
- 14-18 years, girls: 15 mg
- 14-18 years, boys: 11 mg
What are the risk factors for iron deficiency in children?
Infants and children at highest risk of iron deficiency include:
- Babies who are born prematurely — more than three weeks before their due date — or have a low birth weight
- Babies who drink cow's milk or goat's milk before age 1
- Breast-fed babies who aren't given complementary foods containing iron after age 6 months
- Babies who drink formula that isn't fortified with iron
- Children ages 1 to 5 who drink more than 24 ounces (710 milliliters) of cow's milk, goat's milk or soy milk a day
- Children who have certain health conditions, such as chronic infections or restricted diets
- Children ages 1 to 5 who have been exposed to lead
Adolescent girls also are at higher risk of iron deficiency because their bodies lose iron during menstruation.
What are the signs and symptoms of iron deficiency in children?
Too little iron can impair your child's ability to function. However, most signs and symptoms of iron deficiency in children don't appear until iron deficiency anemia occurs. If your child has risk factors for iron deficiency, talk to his or her doctor.
Signs and symptoms of iron deficiency anemia might include:
- Pale skin
- Fatigue
- Slowed growth and development
- Poor appetite
- Abnormally rapid breathing
- Behavioral problems
- Frequent infections
- Unusual cravings for non-nutritive substances, such as ice, dirt, paint or starch
How can iron deficiency in children be prevented?
If you're feeding your baby iron-fortified formula, he or she is likely getting the recommended amount of iron. If you're breastfeeding your baby, follow these supplementation recommendations:
- Full-term infants. Start giving your baby an iron supplement at age 4 months. Continue giving your baby the supplement until he or she is eating two or more servings a day of iron-rich foods, such as fortified cereal or pureed meat. If you breast-feed and give your baby fortified formula and the majority of your baby's feedings are from formula, stop giving your baby the supplement.
- Premature infants. Start giving your baby an iron supplement at age 2 weeks. Continue giving your baby the supplement until age 1. If you breast-feed and give your baby fortified formula and the majority of your baby's feedings are from formula, stop giving your baby the supplement.
Other steps you can take to prevent iron deficiency include:
- Serve iron-rich foods. When you begin serving your baby solids — typically between ages 4 months and 6 months — feed him or her foods with added iron, such as iron-fortified baby cereal, pureed meats and pureed beans. For older children, good sources of iron include red meat, chicken, fish, beans and dark green leafy vegetables.
- Don't overdo milk. Between ages 1 and 5, don't allow your child to drink more than 24 ounces (710 milliliters) of milk a day.
- Enhancing absorption. Vitamin C helps promote the absorption of dietary iron. You can help your child absorb iron by offering foods rich in vitamin C — such as citrus fruits, cantaloupe, strawberries, bell pepper, tomatoes and dark green vegetables.
Should I have my child screened for iron deficiency?
Iron deficiency and iron deficiency anemia are typically diagnosed through blood tests. The American Academy of Pediatrics recommends that all infants be tested for iron deficiency anemia starting between ages 9 months and 12 months and, for those who have risk factors for iron deficiency, again at later ages. Depending on the screening results, your child's doctor might recommend an oral iron supplement or a daily multivitamin or further testing.
Iron deficiency in children can be prevented. To keep your child's growth and development on track, offer iron-rich foods at meals and snacks and talk to your child's doctor about the need for screenings and iron supplements.
-
Newborn feeding basics
A newborn's feeding schedule can be unpredictable. Here's what, when and how to feed your baby.
Feeding a newborn is a round-the-clock commitment. It's also an opportunity to begin forming a bond with the newest member of your family. Consider these tips for feeding a newborn.
1. Stick with breast milk or formula
Breast milk is the ideal food for babies — with rare exceptions. If breastfeeding isn't possible, use infant formula. Healthy newborns don't need water, juice or other fluids.
2. Feed your newborn on demand
Most newborns need eight to 12 feedings a day — about one feeding every two to three hours.
Look for early signs of hunger, such as stirring and stretching, sucking motions and lip movements. Fussing and crying are later cues. The sooner you begin each feeding, the less likely you'll need to soothe a frantic baby.
When your baby stops sucking, closes his or her mouth, or turns away from the nipple or bottle, he or she might be full — or simply taking a break. Try burping your baby or waiting a minute before offering your breast or the bottle again.
As your baby gets older, he or she will take in more milk in less time at each feeding.
3. Consider vitamin D supplements
Ask your baby's doctor about vitamin D supplements for the baby, especially if you're breastfeeding. Breast milk might not provide enough vitamin D, which helps your baby absorb calcium and phosphorus — nutrients necessary for strong bones.
4. Expect variations in your newborn's eating patterns
Your newborn won't necessarily eat the same amount every day. During growth spurts — often at two to three weeks after birth and again at six weeks after birth — your newborn might take more at each feeding or want to be fed more often. Respond to early signs of hunger, rather than keeping a strict eye on the clock.
5. Trust your instincts — and your newborn's
You might worry that your newborn isn't eating enough, but babies usually know just how much they need. Don't focus on how much, how often or how regularly your newborn eats. Instead, look for:
- Steady weight gain
- Contentment between feedings
- By the fifth day after birth, at least six wet diapers and three or more bowel movements a day
Contact the doctor if your newborn isn't gaining weight, wets fewer than six diapers a day or shows little interest in feedings.
6. Consider each feeding a time to bond with your newborn
Hold your newborn close during each feeding. Look him or her in the eye. Speak with a gentle voice. Use each feeding as an opportunity to build your newborn's sense of security, trust and comfort.
7. Know when to ask for help
If you're having trouble breastfeeding, ask a lactation consultant or your baby's doctor for help — especially if every feeding is painful or your baby isn't gaining weight. If you haven't worked with a lactation consultant, ask your baby's doctor for a referral or check with the obstetrics department at a local hospital.
Parenting
-
Baby naps
Baby naps can be a restful time for you and your little one — but the process of getting your baby to sleep during the day can be just the opposite. Understand the basics of baby naps.
How many naps a day does a baby need?
It takes awhile for newborns to develop a sleep schedule. During the first month, babies usually sleep and wake round-the-clock, with relatively equal periods of sleep between feedings.
As babies get older, baby nap times typically lengthen and become more predictable. For example:
- Ages 4 months to 1 year. After the newborn period, your baby will likely nap at least twice a day — once in the morning and once in the early afternoon. Some babies also need a late afternoon nap. Many babies nap a total of three or more hours during the day.
- Age 1 year and older. Around this age your baby will likely drop his or her morning nap and only nap in the afternoon, often for a period of two to three hours. During this transition, consider moving up your baby's naptime and bedtime by a half hour to help him or her adjust. Most children continue taking an afternoon nap until ages 3 to 5.
Remember, however, that every baby is different and baby nap schedules can vary considerably.
What's the best way to put my baby down for a nap?
To ease your baby into nap time:
- Set the mood. A dark, quiet and comfortably cool environment can help encourage your baby to sleep.
- Put your baby to bed drowsy, but awake. Drooping eyelids, eye rubbing and fussiness might be signs that your baby is tired. The longer you wait, the more overtired and fussy your baby might become — and the harder it might be for him or her to fall asleep.
- Avoid holding, rocking or feeding your baby to sleep. Eventually, this might be the only way your baby is able to fall asleep. If your baby tends to fall asleep in your arms after a feeding, do something gentle right afterward — such as changing his or her diaper or reading a short story.
- Be safe. Place your baby to sleep on his or her back, and clear the crib or bassinet of blankets and other soft items.
- Be consistent. Your baby will get the most out of daytime naps if he or she takes them at the same time each day and for about the same length of time. Occasional exceptions are inevitable, of course, and won't harm your baby.
What if my baby sounds fussy after I put him or her down?
It's common for babies to cry when put down for sleep, but most will quiet themselves if left alone for a few minutes. If the crying lasts longer than a few minutes, check on your baby and offer comforting words. Then give him or her time to settle again.
If your baby wakes shortly after you put him or her down for a nap and isn't wet, hungry or ill, try to be patient and encourage self-settling. You might gently pat your baby, offer a massage or breast-feed for a short time.
Also, keep in mind that babies are often active during sleep — twitching their arms and legs, smiling, sucking, and generally appearing restless. It's easy to mistake a baby's stirrings as a sign that he or she is waking up or needs to eat. Instead of picking up your baby right away, wait a few minutes to see if your baby falls back to sleep.
Should I limit the length of my baby's naps?
It depends on how well your baby is sleeping at night.
Some babies confuse their days and nights — sleeping more during the day than at night. One way to set your baby straight is to limit daytime naps — especially those in the late afternoon — to no more than three or four hours each. If your baby is napping for too long at the end of the day, it can make it harder for him or her to fall asleep at bedtime.
What should I do if my baby suddenly resists napping?
Some babies and older children go through periods during which they refuse to nap — even though they still need the rest. If this happens, try adjusting your baby's bedtime. Making bedtime a little earlier or later can sometimes help a baby nap better during the day.
Helping your baby get the right amount of daytime sleep isn't always easy. Don't feel bad if some days are more challenging than others. Remember to look and listen for the signs that your baby is tired and try to keep his or her nap routine consistent.
If you have questions or concerns about your baby's napping schedule, talk to his or her doctor.
-
Baby Sleep
Tired of being awake at all hours with your baby? Use these simple tips to help your little one sleep through the night.
If you haven't had a good night's sleep since your baby was born, you're not alone. Sleepless nights are a rite of passage for most new parents — but don't despair. You can help your baby sleep all night. Honestly!
Developing a rhythm
Newborns sleep 16 or more hours a day, but often in stretches of just a few hours at a time. Although the pattern might be erratic at first, a more consistent sleep schedule will emerge as your baby matures and can go longer between feedings.
By age 3 to 4 months, many babies sleep at least five hours at a time. At some point during a baby's first year — every baby is different — he or she will start sleeping for about 10 hours each night.
Have your baby sleep in your room
Ideally, your baby should sleep in your room with you, but alone in a crib, bassinet or other structure designed for infants, for at least six months, and, if possible, up to one year. This might help decrease the risk of sudden infant death syndrome (SIDS).
Adult beds aren't safe for infants. A baby can become trapped and suffocate between the headboard slats, the space between the mattress and the bed frame, or the space between the mattress and the wall. A baby can also suffocate if a sleeping parent accidentally rolls over and covers the baby's nose and mouth.
Encouraging good sleep habits
For the first few months, middle-of-the-night feedings are sure to disrupt sleep for parents and babies alike — but it's never too soon to help your baby become a good sleeper. Consider these tips:
- Follow a consistent, calming bedtime routine. Overstimulation in the evening can make it difficult for your baby to settle to sleep. Try bathing, cuddling, singing, playing quiet music or reading, with a clearly defined end point when you leave the room. Begin these activities before your baby is overtired in a quiet, softly lit room.
- Put your baby to bed drowsy, but awake. This will help your baby associate bed with the process of falling asleep. Remember to place your baby to sleep on his or her back, and clear the crib or bassinet of blankets and other soft items.
- Give your baby time to settle down. Your baby might fuss or cry before finding a comfortable position and falling asleep. If the crying doesn't stop, check on your baby, offer comforting words and leave the room. Your reassuring presence might be all your baby needs to fall asleep.
- Consider a pacifier. If your baby has trouble settling down, a pacifier might do the trick. In fact, research suggests that using a pacifier during sleep helps reduce the risk of SIDS.
- Keep nighttime care low-key. When your baby needs care or feeding during the night, use dim lights, a soft voice and calm movements. This will tell your baby that it's time to sleep — not play.
- Respect your baby's preferences. If your baby is a night owl or an early bird, you might want to adjust routines and schedules based on these natural patterns.
Keeping it in perspective
Remember, getting your baby to sleep through the night isn't a measure of your parenting skills. Take time to understand your baby's habits and ways of communicating so that you can help him or her become a better sleeper. If you have concerns, talk to your baby's doctor.
-
Bathing
Wonder how to do a baby bath? Here's a step-by-step guide to help you master the basics.
Bathing a slippery newborn can be a nerve-wracking experience. Your baby might not like it much, either. With a little practice, however, you'll both start to feel more comfortable at bath time. Start by learning baby bath basics.
How often does my newborn need a bath?
There's no need to give your newborn a bath every day. Three times a week might be enough until your baby becomes more mobile. Bathing your baby too much can dry out his or her skin. If you're quick and thorough with diaper changes and burp cloths, you're already cleaning the parts that need attention — the face, neck and diaper area.
Is it better to bathe my baby in the morning or at night?
That's up to you. Choose a time when you're not rushed or likely to be interrupted. Some parents opt for morning baths, when their babies are alert. Others prefer to make baby baths part of a calming bedtime ritual. If you bathe your baby after a feeding, consider waiting for your baby's tummy to settle a bit first.
Is a sponge bath good enough?
The American Academy of Pediatrics recommends sponge baths until the umbilical cord stump falls off — which might take a week or two. To give your baby a sponge bath, you'll need:
- A warm place with a flat surface. A bathroom or kitchen counter, changing table, or firm bed will work. Even a blanket or towel on the floor is OK. Pad hard surfaces with a blanket or towel.
- A soft blanket, towel or changing pad. Spread it out for your baby to lie on.
- A free hand. Always keep one hand on your baby. On a changing table, use the safety strap as well.
- A sink or shallow plastic basin to hold the water. Run warm water into the basin or sink. Check the water temperature with your hand to make sure it's not too hot.
- Essential supplies. Gather a washcloth, a towel — preferably with a built-in hood — mild baby shampoo, mild moisturizing soap, baby wipes, a clean diaper and a change of clothes.
Undress your baby and wrap him or her in a towel. Lay your baby on his or her back in the prepared area. To keep your baby warm, only expose the parts of your baby's body you're washing. Wet the washcloth, wring out excess water and wipe your baby's face. Wipe each eyelid, from the inside to the outside corner.
To clean your baby's body, use plain water or a mild, moisturizing soap. Pay special attention to creases under the arms, behind the ears, around the neck and in the diaper area. Also wash between your baby's fingers and toes.
What type of baby tub is best?
Once your baby is ready for a bath, you might use a plastic tub or the sink. Line the tub or sink with a clean towel. Gather the supplies you'd use for a sponge bath, a cup of rinsing water and baby shampoo, if needed, ahead of time. This will allow you to keep one hand on the baby at all times. Never leave your baby alone in the water.
How much water should I put in the tub? A common recommendation is 2 inches (about 5 centimeters) of warm — not hot — water. To keep your baby warm, you can pour warm water over his or her body throughout the bath. Some research suggests that using slightly more water — enough to cover a baby's shoulders — can be calming and help reduce heat loss. With any amount of water, be sure to hold your baby securely during the bath.
What about water temperature?
Warm water is best. To prevent scalding, set the thermostat on your water heater to below 120 F (49 C). Always check the water temperature with your hand before bathing your baby. Aim for bath water around 100 F (38 C). Be sure the room is comfortably warm, too. A wet baby can be easily chilled.
What's the best way to hold my newborn in the tub?
A secure hold will help your baby feel comfortable — and stay safe — in the tub. Use your nondominant arm to support your baby's head and neck and the other to hold and guide your baby's body into the water, feet first. Continue supporting your baby's head and back as needed. You might reach behind your baby and hold on to his or her opposite arm throughout the bath.
What should I wash first?
Most parents start with the baby's face and move down to dirtier parts of the body. This keeps rinsed areas from getting soapy again.
Should I wash my newborn's hair?
If your newborn has hair and you think it needs washing, go ahead. With your free hand gently massage a drop of mild baby shampoo into your baby's scalp. Rinse the shampoo with a cup of water or a damp washcloth, cupping one hand across your baby's forehead to keep suds out of his or her eyes.
Will lotion after a baby bath help prevent rashes?
Most newborns don't need lotion after a bath. If his or her skin is very dry, apply a small amount of unscented baby moisturizer to the dry areas. The massage might make your baby feel good. If dryness continues, you might be bathing your baby too often.
-
Crying Baby: What to do when your newborn cries
Newborn crying jags are inevitable. Here's help soothing a crying baby — and renewing your ability to handle the tears.
The dream: Your baby sleeps through the night after just a few weeks, gurgles happily while you run errands and fusses only when hunger strikes.
The reality: Your baby's favorite playtime is after the 2 a.m. feeding. Crankiness peaks when you're out and about. You had no idea a baby could cry for so long.
Sound familiar? On any given day, a newborn might cry for up to two hours — or even longer. Find out why babies cry, and what to do about it.
Decoding the tears
A crying baby is trying to tell you something. Your job is to figure out why your baby is crying and what — if anything — you can do about it. Consider what your crying baby could be thinking.
I'm hungry
Most newborns eat every few hours round-the-clock. Some babies become frantic when hunger strikes. To avoid such frenzy, respond to early signs of hunger. Frequent burping might help reduce discomfort that could be causing tears.
If you're breastfeeding your baby, the flavor of the milk might change in response to what you eat and drink. If you suspect that a certain food or drink is making your baby fussier than usual, avoid it for several days to see if it makes a difference. If you're feeding your baby formula, your baby's doctor might recommend changing formula.
I want to suck on something
Sucking is a natural reflex. For many babies, it's a comforting, soothing activity. If your baby isn't hungry, you might offer a pacifier or help your baby find his or her finger or thumb.
I'm lonely
Sometimes simply seeing you, hearing your voice or being cuddled can stop the tears. Calmly hold your baby to your chest. You might place your baby on his or her left side to aid digestion or on his or her stomach for support. Gentle pats on the back might soothe a crying baby, too.
I'm tired
Tired babies are often fussy — and your baby might need more sleep than you think. Newborns often sleep up to 16 hours a day. Some newborns sleep even more.
I'm wet
For some babies, a wet or soiled diaper is a surefire way to trigger tears. Check your baby's diaper often to make sure it's clean and dry.
I want to move
Sometimes a rocking session or walk through the house can soothe a crying baby. In other cases, a change of position is all that's needed. Keeping safety precautions in mind, try a baby swing or vibrating infant seat. Head outdoors with the stroller. You might even want to buckle up for a car ride.
I'd rather be bundled
Some babies feel most secure in a swaddle wrap. Snugly wrap your baby in a receiving blanket or other small, lightweight blanket.
I'm hot or cold
A baby who's too hot or cold is likely to be uncomfortable. Add or remove a layer of clothing as needed.
I've had enough
Too much noise, movement or visual stimulation might drive your baby to cry. Move to a calmer environment or place your baby in the crib. White noise — such as a recording of ocean waves or the monotonous sound of an electric fan or vacuum cleaner — might help your crying baby relax.
Over time you might be able to identify your baby's needs by the way he or she is crying. For example, a hungry cry might be short and low-pitched, while a cry of pain might be a sudden, long, high-pitched shriek. Picking up on any patterns can help you better respond to your baby's cries.
Crying it out
If your baby doesn't appear sick, you've tried everything, and he or she is still upset, consider letting him or her cry it out. Crying won't hurt your baby — and sometimes the only way to stop a crying spell is to let it run its course.
Of course, listening to your baby wail can be agonizing. If you need to distract yourself for a few minutes, place your baby safely in his or her crib and take a quick shower, call a friend or make something to eat.
Is it just fussiness, or is it colic?
Some babies have frustrating periods of intense, inconsolable crying known as colic — typically starting a few weeks after birth and improving by age 3 months.
Colic is often defined as crying more than three hours a day, three days a week for three weeks or longer in an otherwise well-fed, healthy baby. The crying might begin suddenly and for no apparent reason. During an episode, your baby might be difficult — or even impossible — to comfort.
What causes colic remains a mystery, and treatment effectiveness varies. If you're concerned about colic, consult your baby's healthcare provider. He or she can make sure your baby is otherwise healthy and help you learn how to care for a colicky baby.
Taking care of yourself
It's tough to listen to your baby cry. But remaining relaxed will make it easier to console your baby. To take the best care of your baby, it's important to take care of yourself, too.
- Take a break. Ask your spouse, partner or another loved one to take over for a while. Even an hour on your own can help renew your coping strength.
- Make healthy lifestyle choices. Eat a healthy diet. Include physical activity in your daily routine. If you can, sleep when the baby sleeps — even during the day. The better rested you are, the better you'll be able to handle a crying baby.
- Remember that it's temporary. Crying spells often peak at about six to eight weeks and then gradually decrease.
- Know when to contact your baby's healthcare provider. If you're concerned about the crying or your baby isn't eating, sleeping or behaving like usual, contact your baby's healthcare provider. He or she can help you tell the difference between normal tears and something more serious.
It's also important to recognize your limits. If your baby's crying is causing you to lose control, put the baby in a safe place — such as a crib — and go to another room to collect yourself. If necessary, contact a family member or friend, your healthcare provider, a local crisis intervention service, or a mental health help line for support.
-
Crying baby? How to keep your cool
It's tough to listen to a crying baby, but you can handle it. Slow down, take a break — and know when to ask for help.
All babies cry, but the tears can take a toll.
When nothing you do soothes your crying baby, you might feel anxious. What if there's something wrong and you miss it? What if you lose control?
Take heart in your ability to care for your baby — and to recognize when you're reaching the end of your rope.
Cover the basics
When your baby cries, start with the basics.
A crying baby might simply need to be fed, burped or changed. Maybe it's time for a nap, a change in position or a session in the rocking chair. Or perhaps your crying baby needs a little more — or a little less — attention.
When the tears won't stop
If your baby seems otherwise OK but the crying continues, do your best to stay calm. Getting tense or upset might only make the crying worse.
Remember, crying doesn't hurt anyone — including the baby.
To stay in control of the situation, you might:
- Keep it quiet. Hold your baby close to you, and quietly sing or talk to your baby. Repeat a calm word or phrase, such as, "You're OK."
- Get moving. Weather permitting, put your baby in the stroller and take a brisk walk. You might even buckle the baby into his or her car seat and take a short drive.
- Think rationally. Remind yourself that it's OK to be frustrated by your baby's crying, but getting angry isn't going to help.
- Take a timeout. If you're alone, put your baby in a safe place — such as the crib or bassinet. Let your baby cry while you take a few minutes to regroup in another room.
- Be realistic. Remind yourself that you're not failing your baby if you can't stop a crying spell. Sometimes babies simply need to cry it out.
- Ask for help. Let your partner or another loved one take over for a while. Take advantage of baby-sitting offers from trusted friends or neighbors. Use the time to take a nap or simply relax. If you're worried about your ability to cope with a crying baby, contact a family member or friend, your healthcare provider, a local crisis intervention service or a mental health help line for support.
Be gentle
When your crying baby can't be calmed, you might be tempted to try just about anything to get the tears to stop. It's OK to be creative — but never shake your baby.
Babies have weak neck muscles and often struggle to support their heads. Shaking your baby out of sheer frustration might have devastating consequences — including blindness, brain damage or mental retardation. Severe shaking can be life-threatening or even fatal.
If you're having trouble managing your emotions or dealing with parenthood, seek help. Your baby's healthcare provider might offer a referral to a counselor or other mental health provider.
-
Maternity leave: Tips for returning to work
Maternity leave passes quickly. Find out what you can do to ease your transition back to work — and how to stay connected to your baby.
Are you dreading the day your maternity leave ends? Don't despair. Working mothers face many challenges, but with some planning you can make your transition back to work a smoother one.
Before you return to work
While you're still on maternity leave, set yourself up for a successful return to work:
- Find dependable child care. Consider local child care providers and facilities or make other arrangements. Look for a safe, stimulating environment and qualified caregivers. Ask your baby's doctor, friends, neighbors and co-workers for recommendations. Check caregivers' references and trust your instincts.
- Talk to your employer. Clarify your job duties and schedule so that you'll know what's expected of you after your maternity leave. You might ask about flexible hours, telecommuting or working part time.
- Prepare to continue breastfeeding. If you plan to breast-feed after returning to work, talk to your employer. Ask about a clean, private room with an outlet for breast pumping. Consider buying or renting an electric pump that allows you to pump both breasts at once.
About two weeks before returning to work, adjust your nursing schedule at home so you're pumping at least once each day and nursing before and after your upcoming work hours. Have someone else feed your baby a bottle of breast milk to help your baby adapt. If you have on-site or nearby child care, consider the logistics of breastfeeding your baby during the workday. - Set a return-to-work date. If you can, go back to work late in the week. That'll make your first week back to work a shorter one.
Once you're back at work
When you go back to work, expect ups and downs as you become more adept at managing multiple demands. These tips can help:
- Get organized. Make a daily to-do list. You might divide the list into tasks for work and tasks for home, or tasks for you and tasks for your partner. Identify what you need to do, what can wait — and what you can skip.
- Provide continuity of care. Develop a good relationship with your baby's caregiver. Spend time talking to him or her when you drop off or pick up your baby. Share family stresses that might affect your baby. Ask about what happened in your absence, such as a change in bowel movements or eating patterns or a new way of playing. Periodically discuss your baby's progress and any concerns.
- Stay connected. Consider a daily phone call or text message to your baby's caregiver to find out how your baby's doing. Place a favorite photo of your baby in your work area. Set aside time after work to reconnect with your baby.
- Make backup plans. Know what you'll do if your baby is sick or your baby's caregiver is unavailable on a workday — such as you or your partner taking the day off, or calling a backup babysitter, friend or loved one to care for your baby.
- Honor your commitment to breastfeeding. Bring your breast pump, containers for expressed milk, an insulated bag and ice packs to work. Keep breast pads handy, in case your breasts leak. If finding time to pump is difficult, consider pumping during breaks or working from home to make up for the lost hours. Try increasing your breastfeeding by feeding your baby in short, frequent sessions just before work and as soon as you return home. You could also pump more on the weekends to increase your supply.
- Seek support. Accept help from your partner, loved ones, friends and co-workers. Speak up if you're feeling guilty, sad or overwhelmed. If you're having trouble pumping milk at work or nursing your baby at home, contact a lactation consultant from a local hospital or clinic.
- Nurture your own well-being. Emotions can run quite high during this time. Your emotional well-being is just as important as taking care of your baby. Relax in the tub after you put the baby to bed, or unwind with a book or music. Cut down on unnecessary commitments. Pick a reasonable bedtime and stick with it. On your days off, sleep when your baby sleeps.
Let go of guilt
Returning to work after maternity leave can pose emotional conflicts for mothers. Remember, there is no such thing as a perfect mother. Working outside the home doesn't make you a bad mother — in fact, studies have not found that children experience any harm when their mothers work outside the home.
It's OK to look forward to the challenges and social aspects of your job. However you balance family and work, aim to be present when you're with your baby. A child who is treated with care and attention will thrive whether or not a mother works.
-
New dad tips
Becoming a new dad can bring joy — and stress. Find out how to deal with the difficulties of parenthood and develop a rewarding relationship with your newborn.
Becoming a father can be an exciting and overwhelming experience. As a new dad, however, you can take steps to prepare for the emotions and challenges of fatherhood and connect with your newly expanded family. Understand how to make your transition to fatherhood less stressful and more fulfilling.
Recognize sources of stress
No one said taking care of a newborn would be easy. As a new dad, you might worry about:
- Limited paternity leave. If you aren't able to take time off when the baby is born, it might be difficult to keep up your regular work schedule and find time to spend with your newborn.
- New responsibilities. Newborns require constant care. On top of feedings, diaper changes and crying spells, parents must find time to do household chores and other activities. This can be stressful for new parents who are used to a more independent lifestyle.
- Disrupted sleep. Newborns challenge their parents' ability to get a good night's sleep. Sleep deprivation can quickly take a toll on new moms and dads.
- Financial strain. The cost of your baby's delivery, healthcare, diapers, clothing and other supplies can add up quickly. The financial strain might be worse if you move to a bigger home or pay someone to take care of the baby while you work — or you or your partner takes unpaid leave or quits work to take care of the baby.
- Less time with your partner. Having a baby means sharing your partner's attention with a third party. It's common for a new dad to feel left out.
- Loss of sexual activity. Recovery from childbirth, physical exhaustion and stress can take a toll on your sex life, which might strain your relationship.
- Depression. Research shows that some fathers — like mothers — experience depression shortly after a child's birth.
Take action before your baby is born
If your partner is still pregnant, ease anxiety by actively preparing for fatherhood. As a new dad, you can:
- Get involved. During pregnancy, men don't experience the same daily reminders that they're about to become parents as do women. Placing your hand on your partner's belly to feel the baby kick, attending prenatal visits and talking about the pregnancy with others can help you feel involved.
- Attend prenatal classes. Prenatal classes can help you and your partner find out what to expect during labor and delivery, as well as learn how to take care of a newborn.
- Consult a financial planner. Talking to a financial planner can help you determine ways to handle the cost of having a baby.
- Build a network of social support. During pregnancy, your partner might get support from healthcare providers, loved ones and friends. It's important for men to have a support network during this time, too. Seek out friends and loved ones who can give you advice and encouragement as you prepare to become a father.
- Talk to your partner. Talk about how your daily lives and relationship might change — for better and for worse — once the baby is born.
- Consider what kind of father you want to be. Think about your own father. Consider what aspects of that relationship you might want to emulate with your own child and what you might do differently.
Stay involved after your baby is born
Once your baby is born, look for ways to connect with your newly expanded family. As a new dad, you can:
- Room with your family at the hospital. If the hospital allows, stay with your partner and newborn until it's time to take the baby home.
- Take turns caring for the baby. Take turns feeding and changing the baby. If your partner is breastfeeding, offer to bottle-feed pumped breast milk — or burp the baby and put him or her to sleep after breastfeeding sessions.
- Play with the baby. Women tend to provide low-key, soothing stimulation for their babies, and men often engage their babies in noisier, more vigorous activities. Both styles of play are important, and seeing your newborn smile can be its own reward.
- Be affectionate with your partner. Intimacy isn't limited to sex. Hugs, kisses and shoulder rubs can help you stay connected while your partner recovers from childbirth and both of you adjust to the new routine. Continue talking to your partner about the changes you're experiencing and how you can support each other as your baby grows.
- Seek help. If you're having trouble dealing with changes in your relationship or you think you might be depressed, talk to a counselor or other mental health provider. Untreated depression affects the entire family.
Becoming a new dad is a life-changing experience. By recognizing and planning for the challenges ahead, you can ease your stress and spend more time enjoying your new family.
-
New sibling: Preparing your older child
A new sibling can have a big impact on your family. Understand how to prepare your older child, introduce the new baby and encourage a healthy sibling bond.
Bringing home a newborn is a little different the second time around. With your first child, you were focused on recovering from childbirth and figuring out how to care for a baby. With the second baby, you're likely to wonder how your older child will react to having a new sibling — and how you're going to meet both of their needs. Here's help making the adjustment.
How can I prepare my older child for a new sibling?
Start by talking to your older child about the arrival of his or her new sibling. Show your older child your growing abdomen and ask him or her to help you set up the baby's nursery. Check into sibling preparation classes at a local hospital.
Explain to your older child that the baby will eat, sleep and cry most of the time. The baby won't be a playmate right away. If your child will need to change rooms or move out of the crib to make space for the new baby, do so before the baby is born. This will give your older child a chance to get used to the new setup before dealing with the baby's arrival.
Try to complete your older child's toilet training before the baby is born or wait until a few months after you bring your baby home to start the process. Arrange for your older child's care during your time in the hospital or birth center, and let your child know what to expect.
How should I introduce my older child to his or her new sibling?
When the new baby arrives, have your partner or a loved one bring your child to the hospital or birth center for a brief visit. Allow another loved one to hold the baby for a while so that you can give your older child plenty of cuddles.
Consider giving your older child a gift that's from the baby, such as a T-shirt that says big brother or big sister. When you're home, take your older child to a special place — such as a favorite playground — to celebrate the new baby's arrival.
What can I do to help my older child adjust to having a new sibling?
Your older child's age and development will affect how he or she reacts to a new sibling. While older children are typically eager to meet a new sibling, younger children might be confused or upset. Consider ways to help your child adjust. For example:
- Children younger than age 2. Young children likely won't understand yet what it means to have a new sibling. Talk to your child about the new addition to your family. Look at picture books about babies and families.
- Children ages 2 to 4. Children at this age might feel uncomfortable sharing your attention with a newborn. Explain the baby will need lots of attention and encourage your older child's involvement by taking him or her shopping for baby supplies. Read to your older child about babies, brothers and sisters. Give your older child a doll so that he or she can be a caregiver, too. Look at your older child's baby pictures together and tell the story of his or her birth.
- School-age children. Older children might feel jealous of how much attention a new baby gets. Talk to your older child about your newborn's needs. Point out the advantages of being older, such as going to bed later. You might display your older child's artwork in the baby's room or ask your older child to help take care of the baby.
Regardless of your older child's age, make sure that he or she gets individual attention when the new baby arrives. If you're taking pictures or videos, include your older child. Take pictures or videos of him or her alone, too. Consider having a few small gifts on hand to give to your older child in case friends visit with gifts for the new baby.
What should I do if my child begins to act out?
Your older child might try to get attention by breaking rules — even if it means being punished. To stop this behavior, praise your older child when he or she is behaving well. If you suspect your child is behaving badly to get attention, consider ignoring the behavior. This might encourage your child to look for a more positive way to get your attention. Talk to your older child. Ask him or her how it feels to have a new sibling. Listen.
Keep in mind that siblings sometimes regress after the arrival of a new baby — such as by having toilet training accidents or drinking from a bottle — to get attention. There's no need to punish this type of behavior. Instead, give your older child love and assurance.
How can I encourage my older child to be gentle with the new baby?
Sometimes older children — stressed by the changes happening around them — take out their frustration on a new baby. If your older child tries to harm the baby, it's time for a talk about appropriate behavior. Also, give your older child extra attention and include him or her in activities that involve the baby, such as singing, bathing or changing diapers. Praise your older child when he or she acts lovingly toward the new baby.
Even if your children seem to get along, supervision is essential. Don't leave your newborn alone with a sibling or other loved one younger than age 12.
How will my older child react to seeing me breast-feed the new baby?
If you plan to breast-feed your newborn, you might wonder how your older child will react or how to keep your older child busy while you nurse. Your older child might hover upon first seeing you breast-feed. Explain what you're doing and answer any questions your child might have. If you breast-fed your older child, explain that you once did the same thing for him or her.
Consider creating a breastfeeding routine that involves your older child. He or she can play a special role, such as helping with a diaper change before the feeding or getting you a pillow. To keep your child entertained while you nurse, set out special toys or a workbook beforehand. Play music or audio versions of children's books. Invite your older child to cuddle with you while you nurse. If your older child asks if he or she can nurse, the decision is up to you. Most older children find the experience somewhat strange and lose interest.
How do I explain a medical concern to my older child?
If your new baby has health issues, explain to your older child that his or her baby sister or brother is sick, and you're worried. If your baby needs to stay in the hospital after he or she is born, ask about the sibling visitation policy. You might also take pictures of the baby and show them to your older child.
Keep in mind that if you don't talk to your older child about the baby's condition, he or she will likely still sense that something is wrong. Rather than keeping your older child in the dark, give him or her some information about the situation and show that you're there for him or her.
A new sibling will undoubtedly change your family. As your older child adjusts, reassure him or her of your love. Explain that he or she has an important role to play now, too — that of big brother or big sister.
-
Newborn care: 10 tips
Round-the-clock newborn care can turn your life upside down. Use these practical strategies to handle the new stress in your life.
A newborn can bring a whirlwind of activity and excitement to your life — and plenty of stress and fatigue, too. Whether you're a first-time parent or a veteran, consider 10 practical tips to keep stress under control.
1. Take care of yourself
Resist the urge to count caffeine as a major food group or a substitute for sleep.
Instead, eat a healthy diet, drink plenty of water and get some fresh air. Sleep when the baby sleeps — and try to work out a nighttime schedule with your partner that allows both of you to rest and care for the baby. Good habits will help you maintain the energy you need to care for your newborn.
2. Establish visiting rules
Friends and loved ones might come out of the woodwork to admire your newborn. Let them know which days work best and how much time you have for a visit.
Insist that visitors wash their hands before holding the baby, and ask anyone who's ill to stay home.
Let trusted visitors care for the baby while you get some much needed rest.
3. Go with the flow
Allow plenty of time each day for nursing sessions, naps and crying spells. Keep scheduled activities to a minimum. When you need to head out, give yourself extra time to pack your supplies and make that inevitable last-minute diaper change.
4. Expect a roller coaster of emotions
You might go from adoring your baby and marveling at tiny fingers and toes to grieving your loss of independence and worrying about your ability to care for a newborn, all in the space of an hour.
Chances are, you and your partner are both tired and anxious as well.
To help you stay connected, talk about what's bothering you — such as a strained budget or difficulty soothing the baby. A shared laugh might help lighten the mood.
5. Relax your standards
Leave dust bunnies where they lie for now. Store clean clothes in the laundry basket — or in stacks on the floor — until you need them. Clean the bathroom with a fresh diaper wipe. Serve cold cereal and peanut butter toast for dinner when you're too tired to prepare a more traditional meal.
6. Get out of the house
If you're going stir-crazy with a fussy newborn, take the baby out for a walk. If you can, let someone you trust take over for a while.
7. Accept a helping hand
When friends and loved ones offer to help, take them up on it. Suggest holding the baby, folding the laundry or running a few errands — whatever would help you the most.
8. Nurture other relationships
Your newborn needs your love and attention, but you won't let your baby down by spending time with others.
If you have other children, set aside one-on-one time with each of them. Schedule dates with your partner. Meet a friend for lunch or a movie.
9. Keep your perspective
The newborn days won't last long. Step back and appreciate the moment, even amid the chaos.
10. Know when to seek additional help
Parenting is a challenge, even on a good day. If you're depressed or you're having trouble adjusting to life with a newborn, consult your healthcare provider or a mental health provider.
Learning to handle the new stress in your life can help you enjoy the riches parenting has to offer.
-
Pacifiers: Are they good for your baby?
The decision to use a pacifier — or not — is up to you. Consider the do's and don'ts of giving your baby a pacifier, and how to help him or her break the habit.
Most babies have a strong sucking reflex. Some babies even suck their thumbs or fingers before they're born. Beyond nutrition, sucking often has a soothing, calming effect. That's why many parents rank pacifiers as must-haves, right up there with diaper wipes.
Are pacifiers really OK for your baby, though? Understand the benefits and risks of pacifier use, important safety tips, and steps to help wean your baby from the pacifier.
The pros
For some babies, pacifiers are the key to contentment between feedings. Consider the advantages:
- A pacifier might soothe a fussy baby. Some babies are happiest when they're sucking on something.
- A pacifier offers temporary distraction. A pacifier might come in handy during and after shots, blood tests or other procedures.
- A pacifier might help your baby fall asleep. If your baby has trouble settling down, a pacifier might do the trick. Pacifier use does not appear to have any impact on a baby's length of sleep or nighttime awakenings.
- A pacifier might ease discomfort during flights. Babies can't intentionally "pop" their ears by swallowing or yawning to relieve ear pain caused by air pressure changes. Sucking on a pacifier might help.
- A pacifier might help reduce the risk of sudden infant death syndrome (SIDS). Sucking on a pacifier at nap time and bedtime might reduce the risk of SIDS. If you're breastfeeding, wait to offer a pacifier until your baby is 3 to 4 weeks old and you've settled into an effective nursing routine.
- Pacifiers are disposable. When it's time to stop using pacifiers, throw them away. If your child prefers to suck on his or her thumb or fingers, it might be more difficult to break the habit.
The cons
Of course, pacifiers have pitfalls as well. Consider the drawbacks:
- Early pacifier use might interfere with breastfeeding. Sucking on a breast is different from sucking on a pacifier or bottle, and some babies are sensitive to those differences. Some research links pacifier use to less frequent breastfeeding or the ending of breastfeeding after only a few months in certain babies. However, a review of unrestricted pacifier use in healthy, full-term infants found that it had no impact on the continuation of breastfeeding.
- Your baby might become dependent on the pacifier. If your baby uses a pacifier to sleep, you might face frequent middle-of-the-night crying spells when the pacifier falls out of your baby's mouth.
- Pacifier use might increase the risk of middle ear infections. However, rates of middle ear infections are generally lowest from birth to age 6 months — when the risk of SIDS is the highest and your baby might be most interested in a pacifier.
- Prolonged pacifier use might lead to dental problems. Normal pacifier use during the first few years of life doesn't cause long-term dental problems. However, prolonged pacifier use might cause a child's teeth to be misaligned or not come in properly.
Pacifier do's and don'ts
If you choose to offer your baby a pacifier, keep these tips in mind:
- Wait until breastfeeding is well-established. If you're breastfeeding, the American Academy of Pediatrics recommends waiting to offer a pacifier until your baby is 3 to 4 weeks old, and you've settled into an effective nursing routine.
- Don't use a pacifier as a first line of defense. Sometimes a change of position or a rocking session can calm a crying baby. Offer a pacifier to your baby only after or between feedings.
- Choose the silicone one-piece, dishwasher-safe variety. Pacifiers made of two pieces pose a choking hazard if they break. Once you've chosen a favorite pacifier, keep a few identical backups on hand.
- Let your baby set the pace. If your baby's not interested in the pacifier, don't force it. If the pacifier falls out of your baby's mouth while he or she is sleeping, don't pop it back in.
- Keep it clean. Before you offer your baby a pacifier, clean it thoroughly. Until your baby is 6 months old and his or her immune system matures, frequently boil pacifiers or run them through the dishwasher. After age 6 months, simply wash pacifiers with soap and water. Resist the temptation to "rinse" the pacifier in your own mouth. You'll only spread more germs to your baby.
- Don't sugarcoat it. Don't put sweet substances on the pacifier.
- Keep it safe. Replace pacifiers often and use the appropriate size for your baby's age. Watch for loose parts or signs of deterioration. Also use caution with pacifier clips. Never attach a pacifier to a string or strap long enough to get caught around your baby's neck.
Pulling the plug
The risks of pacifier use begin to outweigh the benefits as your baby gets older. While most kids stop using pacifiers on their own between ages 2 and 4, others need help breaking the habit. Use praise when your child chooses not to use the pacifier. If your child struggles to give up the pacifier consider talking to your child's doctor or dentist for help.
-
Potty training
Potty training is a major milestone. Get the facts on timing, technique and handling accidents.
Potty training is a big step for kids and parents alike. The secret to success? Timing and patience.
Is it time?
Potty training success hinges on physical, developmental and behavioral milestones, not age. Many children show signs of being ready for potty training between ages 18 and 24 months. However, others might not be ready until they're 3 years old. There's no rush. If you start too early, it might take longer to train your child.
Is your child ready? Ask yourself:
- Can your child walk to and sit on a toilet?
- Can your child pull down his or her pants and pull them up again?
- Can your child stay dry for up to two hours?
- Can your child understand and follow basic directions?
- Can your child communicate when he or she needs to go?
- Does your child seem interested in using the toilet?
If you answered mostly yes, your child might be ready. If you answered mostly no, you might want to wait — especially if your child is about to face a major change, such as a move or the arrival of a new sibling.
Your readiness is important, too. Let your child's motivation, instead of your eagerness, lead the process. Try not to equate potty training success or difficulty with your child's intelligence or stubbornness. Also, keep in mind that accidents are inevitable and punishment has no role in the process. Plan toilet training for when you or a caregiver can devote the time and energy to be consistent on a daily basis for a few months.
Ready, set, go!
When it's time to begin potty training, follow these steps:
- Pull out the equipment. Place a potty chair in the bathroom or, initially, wherever your child is spending most of his or her time. Encourage your child to sit on the potty chair in her clothes to start out. Make sure your child's feet rest on the floor or a stool. Use simple, positive terms to talk about the toilet. You might dump the contents of a dirty diaper into the potty chair and toilet to show its purpose. Have your child flush the toilet.
- Schedule potty breaks. Have your child sit on the potty chair or toilet without a diaper for a few minutes at two-hour intervals, as well as first thing in the morning and right after naps. For boys, it's often best to master urination sitting down, and then move to standing up after bowel training is complete. Stay with your child and read a book or give your child a toy to play with while he or she sits. Allow your child to get up if he or she wants. Even if your child simply sits there, offer praise for trying — and remind your child that he or she can try again later. To maintain consistency, bring the potty chair with you when you're away from home with your child.
- Get there — Fast! When you notice signs that your child might need to use the toilet — such as squirming, squatting or holding the genital area — respond quickly. Help your child become familiar with these signals, stop what he or she is doing, and head to the toilet. Praise your child for telling you when he or she has to go. Keep your child in loose, easy-to-remove clothing.
- Explain hygiene. Teach girls to spread their legs and wipe carefully from front to back to prevent bringing germs from the rectum to the vagina or bladder. Make sure your child washes his or her hands afterward.
- Ditch the diapers. After a couple of weeks of successful potty breaks and remaining dry during the day, your child might be ready to trade diapers for training pants or underwear. Celebrate the transition. Let your child return to diapers if he or she is unable to remain dry. Consider using a sticker or star chart for positive reinforcement.
If your child resists using the potty chair or toilet or isn't getting the hang of it within a few weeks, take a break. Chances are he or she isn't ready yet. Pushing your child when he or she isn't ready can lead to a frustrating power struggle. Try again in a few months.
Nighttime training
Nap and nighttime training typically take longer to achieve. Most children can stay dry at night between ages 5 and 7. In the meantime, use disposable training pants and mattress covers when your child sleeps.
Accidents will happen
To handle accidents:
- Stay calm. Don't scold, discipline or shame your child. You might say, "You forgot this time. Next time you'll get to the bathroom sooner."
- Be prepared. Keep a change of underwear and clothing handy, especially at school or in child care.
When to seek help
If you have questions about potty training or your child is having difficulties, talk to your child's doctor. He or she can give you guidance and check to see if there's an underlying problem.
-
Premature Baby
If you have a premature baby, understand the challenges your preemie might face — and remember the importance of meeting your own needs.
If your baby is born too early, the miracle of birth might be overshadowed by health concerns and the possible long-term effects of prematurity. However, there's much you can do to take care of your premature baby — and yourself — as you look toward the future.
Your preemie's special challenges
A premature (preterm) baby is born before 37 complete weeks of pregnancy. Generally, the earlier a baby is born, the higher the risk of complications.
At first, your premature baby might have little body fat and need help maintaining body heat. He or she might cry only softly and have trouble breathing due to respiratory distress syndrome or bronchopulmonary dysplasia. Feeding your preemie might be a challenge. Yellowing of the skin (jaundice), a low red blood cell count (anemia of prematurity), temporary pauses in breathing (apnea) and infection are possible. Some preemies have an eye disease in which the retina is not fully developed (retinopathy of prematurity).
Premature babies might also experience impaired cognitive skills, motor deficits, or behavioral, psychological or chronic health problems.
Keep in mind that every baby is different. Your baby's doctor or healthcare team can help you understand your baby's health concerns.
Taking care of your preemie
Your preemie's special needs call for special care, probably in a neonatal intensive care unit (NICU). In some cases, a premature baby needs to be transported to a hospital that can provide specialized care. You might feel helpless, but there are many steps you can take to help your baby. For example:
- Find out about your preemie's condition. Uncertainty can be frightening — as can the monitors, respirators and other types of equipment in the NICU. Write down your questions and seek answers when you're ready. The more you know, the better you'll be able to handle the situation.
- Share your observations and concerns. If you notice changes in your preemie's condition, tell your baby's medical team right away.
- Establish your milk supply. Breast milk contains proteins that help fight infection and promote growth. Although your preemie might not be able to feed from your breast or a bottle at first, breast milk can be given in other ways — or frozen for later use. Begin pumping as soon after birth as possible. Aim to pump at least six to eight times a day, round-the-clock. Also, ask your baby's doctor about your baby's need for supplementation — either in the form of breast milk fortifiers, supplemental vitamins, or preterm infant formula.
- Spend time with your baby. Talking and reading to your baby can help you bond. When your baby is ready, cradle him or her in your arms. Hold your baby under your robe or shirt to allow skin-to-skin contact. Learn to feed, change and soothe your preemie. If you're concerned about interfering with IV tubes or monitor wiring, ask for help. Consider personalizing your baby's incubator with a blanket or family pictures.
Taking care of yourself
You're concentrating on your baby now, but remember that you have needs, too. Taking good care of yourself will help you take the best care of your preemie.
- Allow time to heal. You might need more time to recover from the rigors of childbirth than you imagined. Eat a healthy diet, and get as much rest as you can. When your healthcare provider gives you the OK, make time for physical activity, too.
- Acknowledge your emotions. Expect to feel joy, sadness, anger and frustration. You might celebrate successes one day, only to experience setbacks the next. Take it one day at a time. Remember that you and your partner or spouse might react differently. Support each other during this stressful time.
- Take a break. If you leave the hospital before your baby, use your time at home to prepare for your baby's arrival. Your baby needs you, but it's important to balance time at the hospital with time for yourself and the rest of your family.
- Be honest with your baby's siblings. If you have other children, you might explain that their baby sister or brother is sick and you're worried. Reassure your children that the baby's illness isn't their fault. If your children aren't allowed to see the baby in the NICU, show them pictures.
- Accept help. Allow friends and loved ones to care for older children, clean the house or run errands.
- Seek support. Surround yourself with friends and loved ones. Talk with other NICU parents. Join a local support group for parents of preemies, or check out online communities. Seek professional help if you're feeling depressed or you're struggling to cope with your new responsibilities.
Bringing baby home
When it's time to bring your baby home, you might feel relieved, excited and anxious. It might be daunting to leave behind the on-site support of your baby's medical team. Keep in mind that as you spend more time with your baby, you'll better understand how to meet his or her needs and your relationship will grow stronger.
To ease the transition home:
- Understand your baby's needs. Make sure you know how to administer medications, use monitors at home or give your baby supplemental oxygen or other treatments. Schedule follow-up visits with your baby's doctor, and find out whom to call if you have concerns in the meantime.
- Ask about your baby's car seat. Keep in mind that because sitting semireclined in a car seat can increase the risk of breathing problems or a slow heartbeat, your baby might need to be monitored in his or her car seat before hospital discharge. When you have the OK to use a car seat, don't leave your baby unattended in the car seat. In addition, don't place your baby in a backpack or other upright positioning devices — which might make it harder for him or her to breathe — until you talk to your baby's doctor.
- Find out about available resources. Your baby might be at risk of developmental delays or disabilities. Ask your baby's healthcare team about local, state or federal resources that might be available.
To measure your premature baby's development, use his or her corrected age — your baby's age in weeks minus the number of weeks he or she was premature. For example, if your baby was born eight weeks early, at age 6 months your baby's corrected age is 4 months.
You'll always remember your baby's time in the hospital. Now cherish the opportunity to begin making memories at home.
-
Screen time
Screens are everywhere. As a result, controlling a child's screen time has become much harder for parents. To complicate matters, some screen time can be educational for children as well as support their social development.
So how do you manage your child's screen time? Here's a primer on guiding your child's use of screens and media.
Screen time guidelines
The American Academy of Pediatrics discourages media use, except for video-chatting, by children younger than 18 to 24 months. If you want to introduce digital media to children ages 18 to 24 months, make sure it's high quality and avoid solo media use. For children ages 2 to 5, limit screen time to one hour a day of high-quality programming. As your child grows, a one-size-fits-all approach doesn't work as well. You'll need to decide how much media to let your child use each day and what types of media are appropriate.
The problems with screen time
Unstructured playtime is more valuable for a young child's developing brain than is electronic media. Despite the fact that many digital media programs claim to be educational, children younger than age 2 are more likely to learn and remember information from a live presentation than they are from a video.
By age 2, children can benefit from certain types of screen time, such as programming with music, movement and stories. However, passive screen time shouldn't replace reading, playing or problem-solving. Co-view with your child to help your child understand what he or she is seeing and apply it in real life.
Also, it's crucial to monitor the shows your child is watching and the games or apps he or she is playing to make sure they are appropriate. Avoid fast-paced programming, which young children have a hard time understanding, apps with a lot of distracting content, and violent media. Eliminate advertising on apps, since young children have trouble telling the difference between ads and factual information.
As your child grows, keep in mind that too much or poor quality screen time has been linked to:
- Obesity
- Irregular sleep schedules and shorter duration of sleep
- Behavioral problems
- Loss of social skills
- Violence
- Less time for play
Developing screen time rules
In recognition of how ever-present screens have become, the American Academy of Pediatrics recently held a symposium to share practical advice for parents. Experts noted that children are still doing the same things that they've always done — only now they are often doing them virtually. As a result, it makes sense for parents to apply the same rules to children's real and virtual environments. This means playing with your child, teaching kindness, being involved, and knowing your child's friends and what your child does with them.
The experts also suggested that the quality of the media your child is exposed to is more important than the platform or amount of time spent.
Ensuring screen time quality
Not all apps, online games or programs are created equal. To ensure quality screen time, consider these tips:
- Preview programs, games and apps before allowing your child to view or play with them.
- Seek out interactive options that engage your child, rather than those that just require pushing and swiping or staring at the screen.
- Use parental controls to block or filter internet content.
- Make sure your child is close by during screen time so that you can supervise his or her activities.
- Ask your child regularly what programs, games and apps he or she has played with during the day.
- Play a video game or explore a new app with your child.
- When watching programming with your child, discuss what you're watching and educate him or her about advertising and commercials.
Seek out information from organizations such as Common Sense Media to help you determine if a program, game or app is appropriate.
Remember that at some point your child will be exposed to content that you haven't approved beforehand and devices without internet filters. Talk to your child about the possible situations that could come up and the behavior you expect.
Setting screen time limits for older children
Set reasonable limits for your child's screen time, especially if your child's use of screens is hindering his or her involvement in other activities. Consider these tips:
- Prioritize unplugged, unstructured playtime.
- Create tech-free zones or times, such as during mealtime or one night a week.
- Discourage use of media entertainment during homework.
- Set and enforce daily or weekly screen time limits and curfews, such as no exposure to devices or screens 1 hour before bedtime.
- Consider using apps that control the length of time a child can use a device.
- Require your children to charge their devices outside of their bedrooms at night.
- Keep screens out of your child's bedroom.
- Limit your own screen time.
- Eliminate background TV.
Teaching appropriate behavior
Online relationships and social media have become a major part of adolescent life. Experts suggest that it's OK for your teen to be a part of these worlds — as long as he or she understands appropriate behavior. Explain to your teen what's OK and what's not OK, such as sexting, cyberbullying and sharing personal information online. Teach your child not to send or share anything online that he or she would not want the entire world to see for eternity. No matter how smart or mature you feel your child is, monitor his or her online and social media behavior.
Your child is bound to make mistakes using media. Talk to your child and help him or her learn from them. Also, model positive online etiquette yourself.
Managing your child's use of screens and media will be an ongoing challenge. But by developing household rules— and revisiting them as your child grows — you can help ensure a safe and fun experience.
-
Sex education: Talking to toddlers and preschoolers about sex
Sex education often begins with a child's curiosity about his or her body. Here's how to set the stage for sex education — and how to answer your child's questions.
Sex education is a topic many parents would prefer to avoid. If you have a young child, you might think you're off the hook — at least for a while. But that's not necessarily true.
Sex education can begin anytime, though it's best to let your child set the pace with his or her questions.
Early exploration
As children learn to walk and talk, they also begin to learn about their bodies. Open the door to sex education by teaching your child the proper names for his or her sex organs, perhaps during bath time.
If your child points to a body part, simply tell him or her what it is. This is also a good time to talk about which parts of the body are private.
When your child asks questions about his or her body — or yours — don't giggle, laugh or get embarrassed. Take the questions at face value, and offer direct, age-appropriate responses. If your child wants to know more, he or she will ask.
Expect self-stimulation
Many toddlers express their natural sexual curiosity through self-stimulation. Boys may pull at their penises, and girls may rub their genitals. Teach your child that masturbation is a normal — but private — activity.
If your child starts masturbating in public, try to distract him or her. If that fails, take your child aside for a reminder about the importance of privacy.
Sometimes, frequent masturbation can indicate a problem in a child's life. Perhaps he or she feels anxious or isn't receiving enough attention at home. It can even be a sign of sexual abuse.
Teach your child that no one is allowed to touch the private parts of his or her body without permission. If you're concerned about your child's behavior, consult his or her doctor.
Curiosity about others
By age 3 or 4, children often realize that boys and girls have different genitals. As natural curiosity kicks in, you may find your child playing "doctor" or examining another child's sex organs.
Such exploration is far removed from adult sexual activity, and it's harmless when only young children are involved. As a family matter, however, you may want to set limits on such exploration.
Everyday moments are key
Sex education isn't a single tell-all discussion. Instead, take advantage of everyday opportunities to discuss sex.
If there's a pregnancy in the family, for example, tell your child that babies grow in a special place inside the mother. If your child wants more details on how the baby got there or how the baby will be born, provide those details.
Consider these examples:
- How do babies get inside a mommy's tummy? You might say, "A mom and a dad make a baby by holding each other in a special way."
- How are babies born? For some kids, it might be enough to say, "Doctors and nurses help babies who are ready to be born." If your child wants more details, you might say, "Usually a mom pushes the baby out of her vagina."
- Why doesn't everyone have a penis? Try a simple explanation, such as, "Boys' bodies and girls' bodies are made differently."
- Why do you have hair down there? Simplicity often works here, too. You might say, "Our bodies change as we get older." If your child wants more details, add, "Boys grow hair near their penises, and girls grow hair near their vaginas."
As your child matures and asks more-detailed questions, you can provide more-detailed responses. Answer specific questions using correct terminology.
Even if you're uncomfortable, forge ahead. Remember, you're setting the stage for open, honest discussions in the years to come.
-
Single parent? Tips for raising a child alone
Raising a child on your own can be stressful. If you're a single parent, understand how to cope with the pressure, find support and nurture your child.
If you're raising a child on your own, you're in good company. Single-parent families are more common than ever. Know how to manage some of the special challenges single parents experience and what you can do to raise a happy, healthy child.
Common single-parent challenges
Child rearing can be difficult under any circumstances. Without a partner, the stakes are higher. As a single parent, you might have sole responsibility for all aspects of day-to-day child care.
Being a single parent can result in added pressure, stress and fatigue. If you're too tired or distracted to be emotionally supportive or consistently discipline your child, behavioral problems might arise.
Single-parent families also generally have lower incomes and less access to healthcare. Juggling work and child care can be financially difficult and socially isolating. You might worry about the lack of a male or female parental role model for your child, too.
Positive strategies
To reduce stress in your single-parent family:
- Show your love. Remember to praise your child. Give him or her your unconditional love and support. Set aside time each day to play, read or simply sit with your child.
- Create a routine. Structure — such as regularly scheduled meals and bedtimes — helps your child know what to expect.
- Find quality child care. If you need regular child care, look for a qualified caregiver who can provide stimulation in a safe environment. Don't rely on an older child as your only baby sitter. Be careful about asking a new friend or partner to watch your child.
- Set limits. Explain house rules and expectations to your child — such as speaking respectfully — and enforce them. Work with other caregivers in your child's life to provide consistent discipline. Consider re-evaluating certain limits, such as your child's screen time, when he or she shows the ability to accept more responsibility.
- Don't feel guilty. Don't blame yourself or spoil your child to make up for being a single parent.
- Take care of yourself. Include physical activity in your daily routine, eat a healthy diet and get plenty of sleep. Arrange time to do activities you enjoy alone or with friends. Give yourself a "timeout" by arranging for child care at least a few hours a week.
- Lean on others. Work out a carpool schedule with other parents. Join a support group for single parents or seek social services. Call on loved ones, friends and neighbors for help. Faith communities can be helpful resources, too.
- Stay positive. It's OK to be honest with your child if you're having a difficult time, but remind him or her that things will get better. Give your child an age-appropriate level of responsibility rather than expecting him or her to behave like a "little adult." Keep your sense of humor when dealing with everyday challenges.
Be aware that some research has shown that teens in single-parent households have a higher risk of depression and lower self-esteem. Signs and symptoms of depression may include social isolation; feeling sad, alone or unloved; disliking one’s looks; irritability; and a sense of hopelessness. If you see these signs in your child or teen, talk to his or her doctor.
Talking to your child about separation or divorce
Many single-parent families are the result of divorce or separation. If this is the case in your family, talk to your child about the changes you're facing. Listen to your child's feelings and try to answer his or her questions honestly — avoiding unnecessary details or negativity about the other parent. Remind your child that he or she did nothing to cause the divorce or separation and that you'll always love him or her.
A counselor might be able to help you and your child talk about problems, fears or concerns. Try to regularly communicate with your child's other parent about your child's care and well-being to help him or her adapt. Children who fare best in divorce have parents who continue to communicate on co-parenting issues, placing their children's needs above their own desire to avoid the ex-spouse.
Single parenting and dating
If you're dating, consider the impact your new romantic partner will have on your child. Look for a partner who will treat both you and your child with respect. Consider waiting until you've established a solid relationship with someone before introducing him or her to your child.
When you're ready to make the introduction, explain to your child some of your new partner's positive qualities. Don't expect your new partner and your child to become close immediately, however. Give them time to get to know each other, and be clear that the new partner isn't trying to replace the other parent.
Male and female role models
If your child's other parent isn't involved in his or her life, you might worry about the lack of a male or female parental role model in your child's life. To send positive messages about the opposite sex:
- Look for opportunities to be positive. Point out accomplishments or positive characteristics of members of the opposite sex in your family, the community or even the media. Avoid making broad, negative statements about the opposite sex.
- Contradict negative stereotypes about the opposite sex. Share an example of a member of the opposite sex who doesn't fit the stereotype.
- Include in your life members of the opposite sex who aren't romantic partners. Seek out positive relationships with responsible members of the opposite sex who might serve as role models for your child. Show your child that it's possible to have long-term, positive relationships with members of the opposite sex.
Being a single parent can be a challenging but rewarding experience. By showing your child love and respect, talking honestly and staying positive, you can lessen your stress and help your child thrive.
-
Sleep tips for new parents
Being a new parent can be exhausting. Try these strategies to fit more sleep into your days and nights.
It's 2 a.m. and your newborn is crying. Will you ever get a good night's sleep again?
Although life with a newborn is a round-the-clock adventure, don't lose hope. By ages 3 to 4 months, many babies can sleep at least five hours at a time. At some point during your baby's first year, nighttime stretches of 10 hours are possible. In the meantime, a little creativity can help you sneak in as much sleep as possible.
Suggestions for the weary
While there's no magical formula for getting enough sleep, these strategies can help:
- Sleep when your baby sleeps. Silence your phone, hide the laundry basket and ignore the dishes in the kitchen sink. Calls and chores can wait.
- Set aside social graces. When friends and loved ones visit, don't offer to be the host. Instead, ask if they could watch the baby while you take a nap.
- Don't 'bed share' during sleep. It's OK to bring your baby into your bed for nursing or comforting — but return your baby to the crib or bassinet when you're ready to go back to sleep.
- Split duties. If possible, work out a schedule with your partner that allows each of you alternately to rest and care for the baby.
- Give watchful waiting a try. Sometimes, you might need to let your baby cry himself or herself to sleep. Unless you suspect that your baby is hungry or uncomfortable, it's OK to encourage self-soothing. If the crying doesn't stop, check on your baby, offer comforting words and leave the room. Your reassuring presence might be all your baby needs to fall asleep.
When sleep becomes a struggle
Caring for a newborn might leave you so exhausted that you could fall asleep anytime, anywhere — but that's not always the case. If you have trouble falling asleep, make sure your environment is suited for sleep. Keep your bedroom dark, quiet and cool. Avoid nicotine, caffeine and alcohol late in the day or at night. Get regular physical activity — not too close to bedtime, if possible. Also, avoid stimulating light, such as from screens, and noise around bedtime.
Try not to agonize over falling asleep. If you're not nodding off within a reasonable amount of time, get up and do a quiet activity, such as reading, until you feel sleepy. Then try going back to bed.
If you think you have a sleep problem, talk to your doctor. Identifying and treating any underlying conditions can help you get the rest you need. Remember, taking good care of yourself — including getting adequate sleep — will help you take the best care of your baby.
-
Temper Tantrums
Temper tantrums are a normal part of growing up. A Mayo Clinic specialist explains how to respond to temper tantrums — and what you can do to prevent them.
You're shopping with your toddler in a busy department store. He or she has spied a toy that you don't intend to buy. Suddenly you're at the center of a gale-force temper tantrum. Everyone is looking at you.
What's the best response? Why do these emotional meltdowns happen? And can you prevent them? Consider these tantrum tips.
Why do tantrums happen?
A tantrum is the expression of a young child's frustration with the challenges of the moment. Perhaps your child is having trouble figuring something out or completing a specific task. Maybe your child doesn't have the vocabulary or can't find the words to express his or her feelings. Frustration might trigger anger — resulting in a temper tantrum.
If your child is thirsty, hungry or tired, his or her threshold for frustration is likely to be lower — and a tantrum more likely.
Do young children have tantrums on purpose?
Young children don't plan to frustrate or embarrass their parents. For most toddlers, tantrums are a way to express frustration. For older children, tantrums might be a learned behavior. If you reward tantrums with something your child wants — or you allow your child to get out of things by throwing a tantrum — the tantrums are likely to continue.
Can tantrums be prevented?
There might be no foolproof way to prevent tantrums, but there's plenty you can do to encourage good behavior in even the youngest children.
For example:
- Be consistent. Establish a daily routine so that your child knows what to expect. Stick to the routine as much as possible, including nap time and bedtime. Set reasonable limits and follow them consistently.
- Plan ahead. Run errands when your child isn't likely to be hungry or tired. If you're expecting to wait in line, pack a small toy or snack to occupy your child.
- Encourage your child to use words. Young children understand many more words than they're able to express. If your child isn't yet speaking — or speaking clearly — teach him or her sign language for words such as "I want," "more," "drink," "hurt" and "tired." As your child gets older, help him or her put feelings into words.
- Let your child make choices. Avoid saying "no" to everything. To give your toddler a sense of control, let him or her make choices. "Would you like to wear your red shirt or your blue shirt?" "Would you like to eat strawberries or bananas?" "Would you like to read a book or build a tower with your blocks?"
- Praise good behavior. Offer extra attention when your child behaves well. Give your child a hug or tell your child how proud you are when he or she shares or follows directions.
- Avoid situations likely to trigger tantrums. Don't give your child toys that are far too advanced for him or her. If your child begs for toys or treats when you shop, try to steer clear of areas with these temptations. If your toddler acts up in restaurants, choose places that offer quick service.
What's the best way to respond to a tantrum?
Typically, the best way to respond to a tantrum is to stay calm and ignore the behavior. You also might try to distract your child. A different book or a change of location might help. If you can't stay calm and you're at home, leave the room for a minute.
If your child is hitting or kicking someone, hold him or her until he or she calms down.
When your child quiets down, you might say, "Tantrums won't get my attention. If you want to tell me something, you have to use your words."
What if my child becomes destructive or dangerous?
If a tantrum escalates, remove your child from the situation and enforce a timeout:
- Select a timeout spot. Seat your child in a boring place, such as in a chair in the living room or on the floor in the hallway. Wait for your child to calm down. Consider giving one minute of timeout for every year of your child's age.
- Stick with it. If your child begins to wander around before the timeout is over, return him or her to the designated timeout spot. Don't respond to anything your child says while he or she is in timeout.
- Know when to end the timeout. When your child has calmed down, discuss the reason for the timeout and why the behavior was inappropriate. Then return to your usual activities.
Don't use timeouts too much, however, or they won't work.
What about tantrums in public?
If your child has a tantrum in public, ignore the behavior if possible. If your child becomes too disruptive, take him or her to a private spot for a timeout. After the timeout return to the activity — or your child will learn that a tantrum is an effective way to escape a given situation.
When is professional help needed?
As your child's self-control improves, tantrums should become less common. Most children begin to have fewer tantrums by age 3 and a half. If your child is having trouble speaking at an age-appropriate level, is causing harm to himself or herself or others, holds his or her breath during tantrums to the point of fainting, or if tantrums get worse after age 4, share your concerns with your child's doctor.
The doctor will consider physical or psychological issues that could be contributing to the tantrums. Depending on the circumstances, you might be referred to a mental health provider or, in some cases, a school or community program. Early intervention can stem future behavioral problems and help your child succeed both at home and at school.
-
Toddler Parenting Tips
Toddlers are infamous for tantrums and other behavior issues. To encourage listening and cooperation, follow these parenting tips.
Life can be frustrating for toddlers. Though eager to be independent, young children can't always move as swiftly as they'd like or clearly express their needs. They also tend to have trouble dealing with limits, compromise and disappointment. This can lead to tantrums and misbehavior.
But you can teach your toddler to behave well by providing love, clear rules and a degree of routine. Consider these practical parenting tips.
Show your love
Make sure your displays of affection for your child outnumber any consequences or punishments. Hugs, kisses and good-natured roughhousing reassure your child of your love. Praise and attention also can motivate your toddler to follow the rules.
Prioritize rules
Rather than overloading your child with rules from the outset — which might frustrate him or her — prioritize those geared toward safety first and gradually add rules over time. Help your toddler follow the rules by childproofing your home and eliminating some temptations.
Prevent tantrums
It's normal for a toddler to have temper tantrums. To reduce the frequency, duration or intensity of your child's tantrums:
- Know your child's limits. Your child might misbehave because he or she doesn't understand or can't do what you're asking.
- Explain how to follow the rules. Instead of saying, "Stop hitting," offer suggestions for how to make play go more smoothly, such as "Why don't you two take turns?"
- Take 'no' in stride. Don't overreact when your toddler says no. Instead, calmly repeat your request. You might also try to distract your child or make a game out of good behavior. Your child will be more likely to do what you want if you make an activity fun.
- Pick your battles. If you say no to everything, your child is likely to get frustrated. Look for times when it's OK to say yes.
- Offer choices, when possible. Encourage your child's independence by letting him or her pick out a pair of pajamas or a bedtime story.
- Avoid situations that might trigger frustration or tantrums. For example, don't give your child toys that are too advanced for him or her. Avoid long outings in which your child has to sit still or can't play — or bring along an activity. Also know that children are more likely to act out when they're tired, hungry, sick or in an unfamiliar setting.
- Stick to the schedule. Keep a daily routine so that your child will know what to expect.
- Encourage communication. Remind your child to use words to express his or her feelings. If your child isn't speaking yet, consider teaching him or her baby sign language to avoid frustration.
Enforce consequences
Despite your best efforts, at some point your toddler will break the rules. Ignore minor displays of anger, such as crying — but if your child hits, kicks or screams for a prolonged period, remove him or her from the situation. Consider using these parenting tips to encourage your child to cooperate:
- Natural consequences. Let your child see the consequences of his or her actions — as long as they're not dangerous. If your child throws and breaks a toy, he or she won't have the toy to play with anymore.
- Logical consequences. Create a consequence for your child's actions. Tell your child if he or she doesn't pick up his or her toys, you will take the toys away for a day. Help your child with the task, if necessary. If your child doesn't cooperate, follow through with the consequence.
- Withholding privileges. If your child doesn't behave, respond by taking away something that your child values — such as a favorite toy — or something that's related to his or her misbehavior. Don't take away something your child needs, such as a meal.
- Timeout. When your child acts out, get down to his or her level and briefly and calmly explain why the behavior is unacceptable. Encourage your child to try a more appropriate activity. If the poor behavior continues, guide your child to a designated timeout spot — ideally a quiet place with no distractions. Enforce the timeout until your child is calm and can listen to you. Afterward, reassure your child of your love and guide him or her to a positive activity.
Whatever consequences you choose, be consistent. Make sure that every adult who cares for your child observes the same rules and discipline guidelines. This reduces your child's confusion and need to test you.
Also, be careful to criticize your child's behavior — not your child. Instead of saying, "You're a bad boy," try, "Don't run into the street." Never resort to punishments that emotionally or physically harm your child. Spanking, slapping and screaming at a child are never appropriate.
Set a good example
Children learn how to act by watching their parents. The best way to show your child how to behave is to set a positive example for him or her to follow.
Safety
-
Burn Safety
Promote burn safety by taking these important child safety measures.
Burn safety is a foreign concept to most young explorers. In fact, one of the most difficult lessons young children might learn is that some things — such as stoves, radiators and flickering flames — can be painfully hot. If children play with matches or lighters, the threat can extend to the entire family.
Take burn safety precautions to prevent injuries and dangerous situations.
Burn safety at home
Many ordinary things in a home — including bath water, food and electrical outlets — can cause childhood burns. To prevent burns at home:
- Reduce water temperature. Set the thermostat on your hot water heater to below 120 F (48.9 C). Aim for bath water around 100 F (38 C). Check the temperature of bath water with your hand before putting your child in the bath.
- Avoid hot spills. Don't cook, drink or carry hot beverages or foods while holding a child. Keep hot foods and liquids away from table and counter edges. Don't use tablecloths or placemats, which young children can pull down. Turn the handles of your pots and pans toward the rear of the stove and use back burners when possible. Don't leave the stove unattended when you're cooking.
- Establish 'no' zones. Block access to the stove, fireplace, space heaters and radiators. Don't leave a child unattended in a room when these items are in use.
- Keep hot devices out of reach. Store items designed to get hot, such as clothes irons or curling irons, unplugged and out of reach.
- Test food temperature before feeding young children. Be careful with food or liquids warmed in a microwave, which might heat foods unevenly. Never warm a baby's bottle in the microwave.
- Choose a cool-mist humidifier or vaporizer. Cool-mist humidifiers prevent steam burns and hot-water spills.
- Address outlets and electrical cords. Cover unused electrical outlets with safety caps. Inserting a fork, key or other metal object into an outlet could result in an electrical burn. Keep electrical cords and wires out of the way so that children don't chew on them. Replace damaged, brittle or frayed electrical cords. Don't run cords under rugs or carpets.
- Choose fire-resistant fabrics. Check labels to make sure mattresses and pajamas meet federal flammability standards.
Burn safety outdoors
To protect children from outdoor hazards:
- Watch grills and fire pits. Don't let children play near grills, fire pits or campfires.
- Check car seats. Before placing your child in a car seat, check for hot straps or buckles. If you park in direct sunlight, cover the car seat with a towel or blanket.
- Avoid backyard fireworks. Don't let children play with or near fireworks or sparklers.
Fire prevention
To prevent accidental fires:
- Lock up matches and lighters. Store matches and lighters in a locked cabinet or drawer. Teach children that matches and lighters aren't toys.
- Be careful with candles. Keep burning candles out of reach of children, and extinguish candles before leaving the room.
- Take care with cigarettes. Don't smoke in the house — especially in bed. Use large, deep ashtrays. Empty them frequently and douse with water before disposing ashes and cigarettes.
- Use space heaters wisely. Keep space heaters at least 3 feet (about 1 meter) away from bedding, drapes, furniture and other flammable materials. Never leave a space heater on when you go to sleep or place a space heater near someone who's sleeping.
- Keep your fireplace clean. An annual cleaning and inspection of a fireplace and chimney can help prevent a chimney fire.
- Store flammable materials. Store flammable liquids in original containers, out of reach of children and away from open flames such as pilot lights or grills.
Fire emergency plan
To prevent injury if a fire occurs:
- Install fire alarms. Install at least one fire alarm on each floor of your home and near any bedrooms. Keep the alarms clean and test them monthly. Use long-life batteries and change them at least once a year. Replace smoke alarms every 10 years or after the expiration date marked on the device.
- Learn to use a fire extinguisher. Keep a working fire extinguisher in your kitchen and learn how to use it properly. Store it on a wall out of reach of children and near a door, so that you can exit away from a fire if necessary.
- Teach children to stop, drop and roll. Teach children what to do if their clothes catch fire. Stop immediately and do not run; drop to the floor and cover the face with hands; and roll on the floor to put out flames.
- Practice an evacuation plan. Create and practice an evacuation plan with your children. Determine two ways to exit any room in a house. Don't use lockable doorknobs on a child's bedroom. Teach your children to leave a burning building by crawling under the smoke. Determine a meeting place outside, preferably in the front of a house where firefighters can easily find you. If you live in an apartment building, practice using posted emergency exit routes with your children.
-
Car seat safety
Car seat safety isn't child's play. Understand 10 common mistakes parents make when installing and using car seats.
Knowing how to safely buckle up your child as he or she grows can be difficult. Check out 10 common mistakes parents often make when it comes to car seat safety — and how to avoid them.
1. Getting a used car seat without doing your homework
If you're considering a used car seat for your child, make sure the car seat:
- Comes with instructions and a label showing the manufacture date and model number
- Hasn't been recalled
- Isn't expired or more than 6 years old
- Has no visible damage or missing parts
- Has never been in a moderate or severe crash
If you don't know the car seat's history, don't use it.
2. Placing the car seat in the wrong spot
The safest place for your child's car seat is the back seat, away from active air bags. If the car seat is placed in the front seat and the air bag inflates, it could hit the back of a rear-facing car seat — right where your child's head is — and cause a serious or fatal injury. A child who rides in a forward-facing car seat could also be harmed by an air bag.
If it's necessary for a child to travel in a vehicle such as a pickup truck that has only one row of seats, deactivate the front air bags or install a power switch to prevent air bag deployment during a crash.
If you're placing only one car seat in the back seat, install it in the center of the seat — if a good fit is possible — rather than next to a door to minimize the risk of injury during a crash.
3. Using the car seat outside of the car
A car seat is designed to protect your child during travel. It's not for use as a general seat or replacement crib in your home. Sitting in a car seat for lengthy periods poses health risks. It can affect your child's ability to breathe, contribute to the development of a flat spot on the back of your baby's head and worsen gastroesophageal reflux disease (GERD) — a chronic digestive disease. In addition, a child can easily be injured by falling out of an improperly used car seat or while sitting in a car seat that falls from a table.
Although it's essential to buckle your child into a car seat during travel, don't let your child sleep or relax in the car seat for long periods of time out of the car.
4. Incorrectly installing the car seat or buckling up your child
Before you install a car seat, read the manufacturer's instructions and the section on car seats in the vehicle's owners manual. Make sure the seat is tightly secured — allowing no more than 1 inch (2.5 centimeters) of movement from side to side or front to back when grasped at the bottom near the attachment points — and facing the correct direction.
If you're using an infant-only seat or a convertible seat in the rear-facing position, keep these tips in mind:
- Use the harness slots described in the car seat's instruction manual, usually those at or below the child's shoulders. Place the harness straps over your child's shoulders.
- Buckle the harness straps and chest clip, with the chest clip even with your child's armpits. Make sure the straps and clip lie flat against your child's chest and over his or her hips with no slack. If necessary, place tightly rolled small blankets alongside your baby or rolled washcloths between the crotch strap and your baby to create a secure fit.
5. Reclining your child at the incorrect angle
In the rear-facing position, recline the car seat according to the manufacturer's instructions so that your child's head doesn't flop forward. Babies must ride semireclined to keep their airways open. Many seats include angle indicators or adjusters to guide you. Keep in mind that as your child grows, you might need to adjust the angle. Check the manufacturer's instructions for details.
6. Moving to a forward-facing car seat too soon
Resist the urge to place your child's car seat in the forward-facing position just so that you can see him or her in your rearview mirror. Riding rear facing is recommended until a child reaches age 2 or the highest weight — typically at least 35 pounds (about 16 kilograms) — or height allowed by the car seat manufacturer. You can start with a convertible seat, which can be used rear facing and, later, forward facing and typically has a higher rear-facing weight and height limit than does an infant-only seat, or switch from an infant-only seat to a forward-facing car seat as your baby grows.
When your child reaches age 2 or the rear-facing weight or height limit of the convertible seat, you can face the seat forward. When you make the switch:
- Install the car seat in the back seat according to the manufacturer's instructions, using either the seat belt or Lower Anchors and Tethers for Children (LATCH) system.
- Use the tether strap — a strap that hooks to the top of the seat and attaches to an anchor in the vehicle — for extra stability.
- Adjust the harness straps so that they're at or above your child's shoulders and fit snugly.
7. Not removing your child's heavy outerwear
Bulky outerwear and blankets can prevent harness straps from snugly securing your baby. Buckle the harness, and then place a coat or blanket over the harness to keep your baby warm.
8. Moving to a booster seat too soon
Older children need booster seats to help an adult safety belt fit correctly. You can switch from a car seat to a booster seat when your child has topped the highest weight — typically 40 to 80 pounds (18 to 36 kilograms) — or height allowed by the car seat manufacturer. Remember, however, that your child is safest remaining in a car seat with a harness for as long as possible.
9. Incorrectly using a booster seat
Booster seats must be used with a lap and shoulder belt — never a lap-only belt. Make sure the lap belt lies low and snug across your child's upper thighs and that the shoulder belt crosses the middle of your child's chest and shoulder.
10. Transitioning to a safety belt too soon
Most kids can safely use an adult seat belt sometime between ages 8 and 12. Here's how you'll know that your child is ready:
- Your child reaches a height of 4 feet 9 inches (nearly 1.5 meters).
- Your child sits against the back of the seat with his or her knees bent comfortably at the edge of the seat — and can remain that way for the entire trip.
- The lap belt rests flat and snugly across your child's upper thighs, and the shoulder belt rests on the middle of your child's chest and shoulder — not on the neck or face.
Make sure your child doesn't tuck the shoulder belt under his or her arm or behind his or her back. Remember, the back seat is the safest place for children younger than age 13.
If you have questions about child passenger safety laws or need help installing a car seat, participate in a local car seat clinic or inspection event. You can also check with the National Highway Traffic Safety Administration for help finding a car seat inspection station.
-
Disposal of unused pain medications
Don't save your leftover pain pills. Opioids can be deadly to small children. Proper disposal is crucial and may include flushing them down the toilet.
If you've ever had surgery, there's a good chance that you have a partially used bottle of prescription pain medication in one of your bathroom cupboards.
Pain medications known as opioids are often prescribed for a sudden, acute episode of pain that occurs after surgery or a traumatic injury, such as a broken bone.
Many people who have been prescribed opioids hang on to any leftovers, just in case they need them in the future. But this practice can have deadly consequences if children or pets accidentally ingest these drugs.
That's why officials with the U.S. Food and Drug Administration (FDA) recommend that people dispose of leftover opioids as quickly as possible. There are many methods of disposal, including flushing them down the toilet if other options aren't available.
Take-back programs
The U.S. Drug Enforcement Administration (DEA) sponsors take-back programs for prescription medications. Authorized collectors may include local law enforcement agencies, hospitals and pharmacies. Take-back options may include:
- Take-back events. Many communities designate a specific day for people to bring in unused prescription drugs to a central collection point.
- Disposal by mail. Some pharmacies offer mail-back envelopes for prescription drug disposal.
- Collection receptacles. Secure collection receptacles are located in many communities. Call your local law enforcement agency to see if there are any in your community.
Some types of prescription drugs can be disposed of in your household trash. Mixing the medications with used coffee grounds or cat litter is often recommended. But the FDA says that opioids are too dangerous to dispose of within household garbage because even one dose to the wrong person can sometimes be fatal.
Illicit use of opioids
In addition to the risk of harm to children or pets accidentally ingesting them, pain medications containing opioids can be stolen and used to get high. Leftover prescription opioids from friends and relatives can easily be diverted for illicit use.
According to the Centers for Disease Control and Prevention (CDC), nearly half of all opioid overdoses in the United States involve a prescription opioid. In 2015, more than 15,000 people died from overdoses involving prescription opioids.
The most common drugs involved in prescription opioid overdose deaths are methadone, oxycodone (OxyContin, Percocet, others) and hydrocodone (Vicodin, Norco, others).
Flushing is a disposal option
If a take-back program is unavailable and the medication appears on the FDA's "flush list," don't hesitate to flush it down the toilet or sink. Flushing should also be considered when the medication cannot be safely and securely stored until disposal via a take-back program, or when there are risks in waiting to do so.
The FDA's "flush list" includes medications that contain:
- Buprenorphine
- Fentanyl
- Hydrocodone
- Hydromorphone
- Meperidine
- Methadone
- Morphine
- Oxycodone
- Oxymorphone
- Sodium oxybate
- Tapentadol
Some of these medications come in the form of patches that adhere to the skin. Used fentanyl patches can be deadly to small children, so the patches should be flushed as soon as you take them off your skin. Fold the sticky sides together before flushing.
Will flushing drugs harm the environment?
Traces of prescription medications, including opioids, have been found in streams and lakes. But FDA officials say that most of these traces come from the urine and feces of people who are taking these drugs.
Weighed against the known risk of harm that unused opioids present via accidental or illicit use, the potential harm to the environment caused by flushing opioids is believed to be negligible.
-
Fall safety
Curious about fall safety for kids? Precautions at home and on the go can help reduce your child's risk of falls and injuries.
Every parent knows how hard it is to protect a child from injuries related to falling. When a baby learns to walk, preventing falls requires constant supervision. Later, a toddler might tumble while trying to get to the cookie jar — and an older child might slip while rocketing up hardwood stairs in socks. Still, there's plenty you can do to promote fall safety and minimize injuries when falls happen.
Preventing falls at home
Taking basic precautions in these hot spots can help prevent falls at home:
- Windows. Most children 5 years old and younger can fit through a 6-inch opening. To prevent falls from windows, install a stop that prevents windows from opening any further than 4 inches. Alternatively, install window guards that cover the lower part of the window. Other prevention strategies include opening double-hung windows only from the top, moving furniture away from windows, and supervising children in a room with open windows. Don't rely on a window screen to prevent falls.
- Stairs. Install safety gates at the top and bottom of staircases. Put doorknob covers on doors that lead to staircases, such as basement doors. Install lower stair rails that are easier for younger children to reach. Don't leave clutter on stairs.
- Porches and balconies. Don't let a child play unattended on a balcony, porch or fire escape even if there are railings. Lock doors and windows that provide access to these areas.
- Baby furniture and equipment. Use preinstalled safety straps on a changing table or highchair. Select a highchair with a wide base that makes tipping less likely. Don't leave a child unattended on a changing table or in a highchair.
- Beds. Install safety rails on beds for toddlers. Bunk beds should be used for children who are six or older. Safety rails on bunk beds should be on both sides of the bed, and gaps between rails should be 4 inches or less. Use a nightlight near the bunk bed stairs or ladder for safe use at night.
- Other furniture. Don't leave a baby unattended on furniture. Place bassinets or portables car carriers on the floor, rather than on tables, counters, beds or other furniture. Place bumpers or guards on sharp corners of furniture to protect toddlers when they fall.
- Bathtubs. Use a bathmat in tubs to lower the risk of falls. Don't leave your child unattended in a bath. Use a nonslip bathmat and clean up wet floors promptly.
- Baby walkers. The American Academy of Pediatrics recommends not using baby walkers, which can lead to falls. Consider alternatives, such as a stationary walker center or activity center.
- Nightlights. Use a nightlight in your child's bedroom, the bathroom and hallways to prevent falls at night.
Fall safety for kids on the go
When you're out and about, consider taking these precautions:
- Strollers. When shopping for a stroller, look for one with a wide base that is less likely to tip. Always use the safety harness when your baby or toddler is in the stroller. To avoid tipping the stroller, don't hang bags from the handles. Check the weight limit of strollers that have a place for older children to stand in the back.
- Shopping carts. Shopping carts can tip easily. Only put a child in the designated seat and use the safety belt. Don't let your child sit in the basket, stand in the cart or hang from the sides of the cart. An adult should push a cart when a child is in the seat.
- Playgrounds. Seek out playgrounds with shock-absorbing surfaces, such as wood chips, mulch, rubber or sand. Falls on cement, packed dirt and turf are more likely to result in injuries. Steer your child to age-appropriate activities to help prevent falls from equipment.
- Helmets and other protective gear. Always have your child wear a helmet while biking, inline skating, skateboarding or riding scooters. When using skates, a scooter or a skateboard, your child should wear guards for the wrists, elbows and knees.
- Escalators. Hold your child's hand when using an escalator. Watch for loose clothing, shoestrings or shoes such as flip-flops that can cause tripping. Don't let your child sit or play on an escalator. Don't use a stroller on an escalator.
- Watch for slippery surfaces. Encourage your child to approach wet, dark and paved areas with caution in cold temperatures. Make sure your child wears shoes or boots with traction in bad weather. A heavy or bulky coat can provide cushioning in the event of a fall. Teach your child not to run around a swimming pool.
Keeping your child safe from falls takes more than luck. Follow these precautions, and you'll go a long way toward preventing injuries.
-
Infant Choking Prevention
Infant choking is scary, but it's largely preventable. Understand why babies are so vulnerable to choking — and what you can do to prevent infant choking.
Worried about infant choking? Find out the common causes of infant choking and what you can do to help protect your baby from choking hazards.
Why are babies vulnerable to choking?
Choking is a common cause of injury and death in young children, primarily because their small airways are easily obstructed. It takes time for babies to master the ability to chew and swallow food, and babies might not be able to cough forcefully enough to dislodge an airway obstruction. As babies explore their environments, they also commonly put objects into their mouths — which can lead to infant choking.
Sometimes health conditions increase the risk of choking as well. Children who have swallowing disorders, neuromuscular disorders, developmental delays and traumatic brain injury, for example, have a higher risk of choking than do other children.
What are the most common causes of infant choking?
Food is the most common cause of infant choking. However, small objects, parts from toys and certain types of behavior during eating — such as eating while distracted — also can cause infant choking.
What can I do to prevent infant choking?
To prevent infant choking:
- Properly time the introduction of solid foods. Introducing your baby to solid foods before he or she has the motor skills to swallow them can lead to infant choking. Wait until your baby is at least 4 months old to introduce pureed solid foods.
- Don't offer high-risk foods. Don't give babies or young children hot dogs, chunks of meat or cheese, grapes, raw vegetables, or fruit chunks, unless they're cut up into small pieces. Don't give babies or young children hard foods, such as seeds, nuts, popcorn and hard candy that can't be changed to make them safe options. Other high-risk foods include peanut butter, marshmallows and chewing gum.
- Supervise mealtime. As your child gets older, don't allow him or her to play, walk or run while eating. Remind your child to chew and swallow his or her food before talking. Don't allow your child to throw food in the air and catch it in his or her mouth or stuff large amounts of food in his or her mouth.
- Carefully evaluate your child's toys. Don't allow your baby or toddler to play with latex balloons — which pose a hazard when uninflated and broken — small balls, marbles, toys that contain small parts or toys meant for older children. Look for age guidelines when buying toys and regularly examine toys to make sure they're in good condition.
- Keep hazardous objects out of reach. Common household items that might pose a choking hazard include coins, button batteries, dice and pen caps.
What should I do if my baby chokes?
If your baby is choking and can't breathe:
- Assume a seated position. Hold the infant face down on your forearm, which is resting on your thigh.
- Thump the infant gently but firmly five times on the middle of the back using the heel of your hand. The combination of gravity and the back blows should release the blocking object.
- Hold the infant face up on your forearm with the head lower than the trunk if the above doesn't work. Using two fingers placed at the center of the infant's breastbone, give five quick chest compressions.
- Repeat the back blows and chest thrusts if breathing doesn't resume. Call for emergency medical help.
- Begin infant CPR if one of these techniques opens the airway but the infant doesn't resume breathing.
To be prepared in case of an emergency take a class on cardiopulmonary resuscitation (CPR) and choking first aid for children. Encourage everyone who cares for your child to do the same.
-
Lead exposure: Tips to protect your child
Don't allow lead exposure to harm your child's health and development. Know the common sources of lead exposure and how to avoid them.
Young children are at the greatest risk of health problems related to lead exposure, including serious brain and kidney damage. Children age 3 and under are especially vulnerable because their ways of playing and exploring — such as crawling and putting objects in their mouths — increase their risk of contact with lead, and of lead entering their bodies through breathing or swallowing.
What are the common causes of lead exposure?
Children can be exposed to lead through many sources, including:
- Prenatal exposure. Lead crosses the placenta. A newborn typically has a blood-lead concentration level similar to his or her mother's.
- Soil and water. Lead particles from a gasoline additive or paint can settle on soil and last for years, and lead and copper pipes soldered with lead can release particles into tap water.
- Lead paint. The use of lead-based paints for homes, children's toys and household furniture has been banned in the United States since 1978. However, lead-based paint is still on walls and woodwork in many older homes and apartments, which can result in children eating lead-based paint chips.
Glazes found on ceramics, china and porcelain also can contain lead, which leaches into food. Lead-based paint may be found in toys and other products produced abroad. - Children's products. Lead may be found in children's jewelry or products made of vinyl or plastic, such as bibs, backpacks, car seats and lunch boxes. A child can absorb lead found in these products by mouthing or chewing on them or can inhale lead if the product is burned, damaged or deteriorating.
- Household dust. Household dust can contain lead from paint chips or soil brought in from outside.
- Food. Food can be contaminated with lead during production, processing, packaging, preparation or storage. For example, vegetables may be grown in soil that contains lead, or exposed to exhaust from fuel that contains lead. Lead can leak into canned foods from tins manufactured with lead solder. And some food containers and pots contain lead, such as lead-glazed pottery and leaded crystal glassware.
- Folk or home health remedies and certain cosmetics. Some traditional remedies, such as the indigestion treatments azarcon and greta, may contain lead. Also, some types of paints and pigments used in makeup and hair dye contain lead.
- Artificial athletic fields. Artificial turf made of nylon or a nylon and polyethylene blend may contain unhealthy levels of lead dust, which could be inhaled or ingested by a child.
How can I protect my child from lead exposure?
You can take simple measures to minimize your child's risk of lead exposure. For example:
What you can do at home
- Check your house. Homes built before 1978 are most likely to contain lead. Professional cleaning, proper paint stabilization techniques and repairs done by a certified contractor can reduce lead exposure.
Be sure to protect your family and belongings while lead issues are being addressed. Before you buy a home, have it inspected for lead. Before you sign a lease, ask the landlord about lead. - Keep children out of potentially contaminated areas. Don't allow your child near old windows, old porches, bare soil, dirt next to an old home, or areas with chipping or peeling paint as well as old window putty that is flaking or chipping.
If possible, lay sod on areas of bare soil or cover bare spots with grass seed, mulch or wood chips. If your home contains chipping or peeling paint, clean up chips immediately and cover peeling patches with duct tape or contact paper until the paint can be removed. -
Filter water. Ion exchange filters, reverse osmosis filters and distillation can effectively remove lead from water. If you don't use a filter and live in an older home, run cold tap water for 15 to 30 seconds before using it.
Use cold tap water for cooking, drinking or making baby formula. Hot water absorbs lead more quickly than does cold water. - Take precautions in the kitchen. Store food in glass, plastic or stainless steel containers — not open cans. If you're not sure if pottery has a lead glaze, use it only for decoration.
- Keep your home clean. Regularly wipe floors and other surfaces with a damp mop or sponge.
- Encourage good hygiene. Make sure your child washes his or her hands and face after playing outside or with pets and before eating and sleeping. Also, regularly wash children's toys, which may become contaminated from soil or household dust.
- Avoid traditional remedies and certain cosmetics. If you're not sure if a traditional remedy or cosmetic contains lead, don't allow your child to use it.
- Promote a balanced diet. Eating a diet high in iron and calcium may decrease a child's absorption of lead.
Tips for at work or play
- Avoid certain children's products and toys. Avoid buying nonbrand toys, old toys, and toys from discount shops or private vendors — unless you can be sure that the toys have been produced without lead or other harmful substances.
Don't give costume jewelry to young children. Regularly check lead recall lists, and keep in mind that commercial lead test kits may not be reliable. - Take precautions around artificial athletic fields. Don't allow your child to eat on an artificial field, and keep drinking containers — when not in use — in a bag or covered container. After leaving the field, have your child remove his or her clothes and turn them inside out to avoid tracking contaminated dust from the play area.
If clothing can't be removed, have your child sit on a towel or blanket in your vehicle. Wash contaminated clothing, towels and blankets separately. Have your child bathe with soap and water after playing on the field.
Keep shoes worn on the field outside of your home. Ideally, remove all shoes when you enter the house and wear no shoes inside or use house slippers indoors. - Take precautions after working with lead. After working with lead, change your clothes and shoes and take a shower. Keep contaminated clothing in the work area or wash your work clothing — separately — as soon as possible.
Also, keep materials used for hobbies that may involve lead, such as ceramics making, away from children and areas where they spend time.
If you think your child has been exposed to lead, ask your child's doctor about a blood test to check for lead.
-
Stroller Safety
Stroller safety starts with choosing the right stroller for your baby. Know what to consider when looking for a stroller and how to keep your baby safe on the go.
If you're like most parents, you'll likely get at least one stroller for your baby. With so many designs and types of strollers, however, how do you choose? Understand how to pick the best stroller for your baby and important stroller safety tips.
What should I consider when looking for a stroller?
When looking at strollers for your baby, consider:
- Your location. If you live in or near a city, you'll likely need a sturdy stroller to maneuver along sidewalks. You might also need to be able to collapse your stroller in a pinch to get on a bus or subway. Suburban parents might want a stroller that's easy to fold and fits into the trunk of a vehicle.
- Your family. If you have an older child, you might want a double stroller or a stroller with an attachment for an older child. If you'll be using an attachment, be sure to read the manufacturer's weight guidelines.
- Your lifestyle. An umbrella stroller might be useful for running errands or traveling. Plan to take your baby along on your runs? You might look for a jogging stroller, too.
- Accessories. Do you want your baby's stroller to have a storage basket, rain cover, blanket, sun shade or cup holder? Some strollers aren't compatible with certain accessories.
What type of stroller is safe for a newborn?
If you plan to use a stroller for your newborn, make sure that the stroller reclines — since newborns can't sit up or hold up their heads. Some strollers fully recline or can be used with a bassinet attachment or an infant-only car seat. Most umbrella strollers, however, don't provide adequate head and back support for young babies.
Also, most jogging strollers aren't designed to recline. As a result, they aren't appropriate for babies until about age 6 months.
What do I need to know about travel systems?
If you have a car, you might look for a stroller that can hold your baby's car seat. Some car seats and strollers come in matching sets, while others require separate attachments that allow the strollers to be used with certain car seats. Once you strap your baby into his or her car seat, these kinds of strollers will allow you to easily move your baby between the stroller and car.
If you use a travel system that allows you to move your baby's car seat from your vehicle to a stroller base, you might be tempted to let your baby finish car naps in the car seat. However, research suggests that sitting upright in a car seat might compress a newborn's chest and lead to lower levels of oxygen in the blood. Even mild airway obstruction can impair a child's development. Experts suggest not letting your child sleep or relax in the car seat for more than two hours.
Sitting in a car seat for lengthy periods can also contribute to the development of a flat spot on the back of your baby's head, as well as worsen any gastroesophageal reflux disease (GERD) — a chronic digestive disease.
What if my baby has special needs?
If your baby was born prematurely or has health concerns, you might want a stroller with storage that will help you carry any necessary equipment, such as a cardiac monitor or oxygen. Parents of babies who have similar health concerns might be a good source of advice.
What other features should I look for?
Consider checking for safety features, including:
- Practical brakes. Look for a stroller that has brakes that are easy to operate. Some strollers have brakes that lock two wheels — a special safety feature. Make sure your baby can't reach the brake release lever.
- A wide base. Strollers that have wide bases are less likely to tip over.
- A single footrest. If you're looking for a side-by-side double stroller, choose one with a single footrest that extends across both sitting areas. Small feet can get trapped between separate footrests.
How can I keep my baby safe in his or her stroller?
To prevent stroller accidents:
- Stay close. Don't leave your baby unattended in his or her stroller.
- Be careful with toys. If you hang toys from a stroller bumper bar to entertain your baby, make sure that the toys are securely fastened.
- Buckle up. Always buckle your baby's harness and seat belt when taking him or her for a stroller ride.
- Use your brakes. Engage your stroller brakes whenever you stop the stroller.
- Properly store belongings. Don't hang a bag from the stroller's handle bar, which can make a stroller tip over.
- Take caution when folding. Keep your baby away from the stroller as you open and fold it, since small fingers can get caught in stroller hinges. Always make sure the stroller is locked open before you put your child in it.
- Keep it out of the sun. During hot weather, don't let your baby's stroller sit in the sun for long periods of time. This can cause plastic and metal pieces to become hot enough to burn your baby. If you leave the stroller in the sun, check the stroller's surface temperature before placing your baby in the stroller.
- Check for recalls. Return the stroller warranty card so that you'll be notified in case of a recall. If you're considering a used stroller, make sure the stroller hasn't been recalled.
-
Swimming: Keep health risks at bay
Kids' swimming: Keep health risks at bay A little preparation can go a long way when it comes to children and water play. Follow these year-round tips for kids' swimming.
Is it OK for your diaper-clad toddler to splash in the local pool? Can your child safely wear a cast or ear tubes in the water? Could bacteria lurking in the pool or lake make your little one sick?
Before you help your child suit up, consider these practical tips from Jay L. Hoecker, M.D., an emeritus pediatrics specialist at Mayo Clinic in Rochester, Minnesota.
Can babies or toddlers wear diapers in the water?
Swim diapers and swim pants are water-repellent and fit snugly around a child's thighs and waist, but they're not waterproof. If your child has a bowel movement in the water, fecal material might escape the diaper.
A dirty diaper might contain diarrhea-causing germs, including the parasite cryptosporidium — which can contaminate pool water or other swimming areas. In otherwise healthy people, a cryptosporidium infection causes diarrhea. The consequences can be more severe for people who have weak immune systems.
Urine in the water is less risky than feces, but it's difficult to separate the two when children wear diapers. If you allow your child to swim in a diaper, take breaks to change the diaper in the bathroom or use the toilet. Don't allow swimming if your child has diarrhea.
Is it risky for children to swallow pool water?
Your child is bound to gulp pool water at one time or another, especially when first learning to swim. A little swallowed pool water isn't typically a cause for concern, but too much pool water can lead to illness. Encourage your child to spit out any water that gets in his or her mouth.
Can children who have casts go swimming?
It depends on the type of cast:
- Plaster cast. If your child has a plaster cast over cloth wrapping, he or she must stay out of the water. Trying to protect a plaster cast with plastic bags generally isn't effective.
- Fiberglass cast. If your child has a fiberglass cast that's lined with a water-repellent liner, it's usually OK to swim — as long as you have the doctor's OK. After swimming, it's important to thoroughly rinse the inside of the cast with clean water. Generally, you can allow the cast to air-dry.
Can children swim if they have ear tubes?
If your child has ear tubes — tiny cylinders placed through the eardrum to drain fluid and allow air into the middle ear — ask his or her doctor about ear protection during swimming. Some doctors recommend that children who have ear tubes wear earplugs while swimming to prevent bacteria from entering the middle ear. However, routine use of earplugs might only be needed when children dive or swim in untreated water, such as lakes and rivers.
What's the best way to prevent swimmer's ear?
Swimmer's ear is an infection that's often treated with prescription eardrops. To prevent swimmer's ear:
- Keep ears dry. Encourage your child to wear earplugs while swimming. After swimming, dry your child's ears by wiping the outer ears gently with a soft towel or use a hair dryer. Put the hair dryer on the lowest setting and hold it at least a foot (about 30 centimeters) away from the ear.
- At-home preventive treatment. If your child doesn't have punctured eardrums, use homemade preventive eardrops before and after swimming. A mixture of 1 part white vinegar to 1 part rubbing alcohol might help promote drying and prevent the growth of bacteria and fungi that can cause swimmer's ear. Pour 1 teaspoon (about 5 milliliters) of the solution into each ear and let it drain back out. Similar over-the-counter solutions might be available at your drugstore.
- Avoid putting foreign objects in your child's ear. Don't use cotton swabs in your child's ears, which can pack material deeper into the ear canal, irritate the thin skin inside the ear or break the skin.
What about red eyes after swimming?
Exposure to chlorine might leave your child with red eyes. To ease discomfort and reduce redness after swimming, rinse your child's eyes with a sterile eyewash or an artificial tears solution. To prevent red or puffy eyes, encourage your child to wear goggles while swimming.
What's the best age to begin swimming lessons?
Many kids learn to ride a bike and to swim on their own at the same age — often the summer before kindergarten. The American Academy of Pediatrics supports swimming lessons for most children age 4 and older.
If you enroll a child younger than age 4 in a swimming program, pick one that requires parental involvement, has qualified teachers and a fun atmosphere, and involves a limited number of underwater submersions. This will limit the amount of water your child might swallow.
Can children swim when they're sick or have cuts and scrapes?
It's fine for children who have colds or other minor illnesses to swim, as long as they feel well enough to do so. Likewise, it's OK for children to swim with cuts and scrapes — as long as the wounds aren't bleeding.
Is it OK to swim right after eating?
It's OK to swim immediately after a light meal or snack. If your child feels lethargic after eating a heavy meal, however, encourage him or her to take a break before swimming.
Are hot tubs safe for children?
Young children can quickly become overheated in a hot tub or spa. The Centers for Disease Control (CDC) do not recommend children under 5 years use a hot tub or spa. If you allow your child to use a hot tub or spa, keep the visit supervised and brief, and don't allow your child to put his or her head underwater. Long hair can get caught in an uncovered hot tub grate and cause drowning.
-
Water Safety
Water can be fun for children to play with — but it can also be deadly. Consider these water safety tips for pools, natural bodies of water and household hazards.
Most children are drawn to water. It's sparkly. Things float in it. It's fun to splash. But water safety is no laughing matter. Anyone can have a water-related accident — even children who know how to swim. To keep your children safe in and near the water, follow these guidelines.
General water safety
To reduce the risk of drowning in any swimming environment:
- Learn cardiopulmonary resuscitation (CPR). Parents and child care providers should know CPR.
- Supervise. Never leave children unsupervised near a pool, hot tub or natural body of water. During gatherings, adults who know how to swim can take turns being the "designated watcher," who isn't distracted. Children under age 4 should be supervised at arm's length, even if they can swim. Don't rely on air-filled or foam toys, such as water wings, noodles or inner tubes, to keep children safe.
- Teach children to swim. According to the American Academy of Pediatrics, most children age 4 and older can learn to swim. Children ages 1 to 4 might be able to learn depending on their physical and emotional development. Swimming lessons, however, don't necessarily prevent drowning and aren't a substitute for adult supervision.
- Avoid alcohol. Don't drink alcohol when you are boating, swimming or supervising children who are swimming.
Residential swimming pools and spas
To ensure water safety in a home pool or spa:
- Fence it in. Install a fence at least 4 feet (1.2 meters) tall that separates the pool area from the house and yard. The fence shouldn't block the view of the pool from outside the fenced area. Vertical slats on fences should have gaps no wider than 4 inches (10.2 centimeters), and the fence shouldn't be more than 4 inches off the ground. Avoid fences that children can easily climb. Install self-closing and self-latching gates that open away from the pool area with latches beyond a child's reach.
- Install alarms. Use an alarm on the house door that leads to the pool area, a floating pool-alarm or a below-water alarm. Keep in mind that an alarm isn't a substitute for appropriate fencing and supervision.
- Block pool and hot tub access. Use a rigid, motorized safety cover to block access to the pool when it's not in use. Secure a cover on hot tubs. Don't allow water to collect on top of the pool or hot tub cover. Remove above-ground pool steps or ladders or lock them behind a fence when the pool isn't in use. Empty inflatable pools after each use.
- Remove toys. Don't leave pool toys in the water. A child might fall into the water while trying to retrieve a toy.
- Beware of drains. Don't allow children to play near or sit on pool or hot tub drains. Body parts and hair can become entrapped by the strong suction. Specially designed drain covers, safety vacuum-release systems and multiple drains can prevent entrapment.
- Keep emergency equipment handy. Equipment might include a life ring with rope, reaching pole or shepherd's crook. Always have a phone in the pool area. If you have a pool or hot tub, follow all local safety ordinances.
Natural bodies of water
Swimming conditions can be unpredictable in ponds, lakes, rivers and oceans. Water depth can change rapidly, as can water temperature, currents and the weather. Murky water might conceal hazards. Follow these water safety tips:
- Wear a life jacket. Children and adults should wear personal flotation devices whenever riding in a boat or fishing. An air-filled swimming aid isn't a substitute for a life jacket.
- Feet first. The first descent into any body of water should be a jump — feet first. Before the jump, check water depth and temperature and look for underwater hazards.
- Stay in designated areas. At public beaches, swim only in areas set aside for swimming. Pay attention to posted warnings about unsafe swimming conditions. Don't allow children to swim in drainage ditches, abandoned surface mines or other water-filled areas not intended for swimming.
- Beware of thin ice. Drowning can occur in the winter, too. Avoid walking, skating or riding on weak or thawing ice. Pay attention to posted warnings regarding ice safety and consult a local department of recreation for current ice conditions. If you spend time on frozen lakes or rivers in winter, learn rescue techniques, such as staying off the ice and using a rope, branch or other long object to reach someone who has fallen through the ice.
Toilets, bathtubs and buckets
A baby can drown in just 1 inch (2.5 centimeters) of water. A curious toddler can fall into a toilet, bucket or fish tank. Consider these precautions:
- Keep the bathroom door closed. Install a safety latch or doorknob cover on the outside of the door.
- Supervise bath time. Never leave a child alone in the bathtub or in the care of another child. Drain water from the tub immediately after use.
- Shut toilet lids. Consider installing childproof locks on lids.
- Store buckets safely. Empty buckets and other containers immediately after use. Don't leave them outside, where they might accumulate water.


