
issues control your life.
Gastroenterology & Hepatology (Digestive Care)
Tests and Procedures
You can benefit from these tests and procedures performed by our gastroenterologists in Osseo:
-
Capsule Endoscopy

Overview
This procedure uses a tiny wireless camera to take pictures of your digestive tract. The camera sits inside a vitamin-sized capsule that is swallowed. As the capsule travels through your digestive tract, the camera takes thousands of pictures that are transmitted to a recorder you wear on a belt around your waist or over your shoulder.
Why it's done
It is used to diagnose diseases of the small intestine including Crohn's disease, celiac disease and other malabsorption disorders; benign and malignant tumors of the small intestine; vascular disorders; and medication-related small bowel injury.
-
Colonoscopy
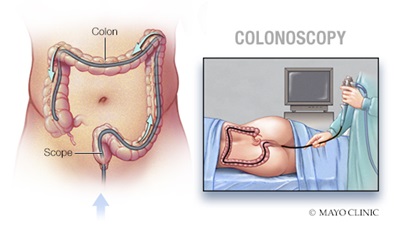
Overview
A colonoscopy is an exam used to detect changes or abnormalities in the large intestine (colon) and rectum. If necessary, abnormal growths called polyps can be removed during a colonoscopy.
Why it's done
Your doctor may recommend a colonoscopy to:
- Investigate certain worrisome signs and symptoms
A colonoscopy can help your doctor explore possible causes of rectal bleeding, chronic diarrhea, iron deficiency anemia , etc. - Colon cancer screening
If you're age 45 or older and at average risk of colon cancer — you have no colon cancer risk factors other than age — or your last colonoscopy was normal 10 years ago, your doctor may recommend a colonoscopy every 10 years to screen for colon cancer. - Colon cancer and polyp surveillance
If you have had polyps before, your doctor may recommend a follow-up colonoscopy to look for and remove any new polyps. This is done to reduce your risk of colon cancer.
Watch a short video on how a colonoscopy is performed:
- Investigate certain worrisome signs and symptoms
-
Endoscopic Mucosal Resection
Overview

Endoscopic mucosal resection (EMR) is a procedure to remove large polyps and very early-stage cancer from the lining of the digestive tract. It can also be used to help determine if a cancer has spread to tissues beneath the digestive tract lining. Endoscopic mucosal resection is performed with a long, narrow tube equipped with a light and video camera. During EMR of the upper digestive tract, the doctor passes this tube (endoscope) down your throat into your esophagus, stomach or upper part of the small intestine (duodenum). To reach the colon, the doctor guides the tube up through the anus. The doctor then inserts instruments through the tube to perform the procedure.
Why it's done
Endoscopic mucosal resection is a less invasive alternative to surgery for removing abnormal tissues from the lining of the digestive tract. Your doctor may recommend the procedure to remove certain early-stage cancers or precancerous growths.
Some of the conditions that EMR has been used to treat include:
- Barrett's esophagus
- Cancer of the small intestine (duodenum)
- Colon polyps
- Colorectal cancer
- Esophageal cancer
- Stomach (gastric) cancer
-
Endoscopic Retrograde Cholangiopancreatography
Overview
Endoscopic retrograde cholangiopancreatography (ERCP) is a procedure that examines the ducts that drain the liver, gallbladder and pancreas. The test combines the use of a flexible, lighted scope (endoscope) with X-ray pictures. It is used to provide important information that cannot typically be obtained by other diagnostic examinations, such as an abdominal ultrasound, CT scan or MRI.
Why it's done
ERCP may be used to remove or crush bile duct and pancreatic duct stones, as well as treat obstructive jaundice (bile duct blockage caused by tumor or stone).
-
Endoscopic Ultrasound
Overview
Endoscopic ultrasound (EUS) is a minimally invasive, using a special endoscope and high-frequency sound waves to produce detailed images of the lining and walls of your digestive tract and chest, nearby organs such as the pancreas and liver, and lymph nodes. When combined with a procedure called fine-needle aspiration, EUS allows your doctor to sample (biopsy) fluid and tissue from your abdomen or chest for analysis. EUS with fine-needle aspiration can be a minimally invasive alternative to exploratory surgery.
Why it's done
EUS is used to further evaluate findings from imaging tests such as a CT scan or MRI. EUS may help in the evaluation of lymphoma, pancreatitis, sarcoidosis, neuroendocrine tumors, and cancers of the esophagus, lung, pancreas, ampulla and rectum.
-
FibroScan®
Overview
FibroScan® is a quick, noninvasive alternative to liver biopsy that helps assess liver health in just 5 to 10 minutes. Using a specialized ultrasound probe placed on the skin, FibroScan® sends painless sound waves through the liver. The speed at which these waves travel provides important information about liver stiffness, which can indicate scarring (fibrosis) or fat buildup (steatosis).
Why it's done
FibroScan® is used to evaluate and monitor liver conditions such as fatty liver disease, hepatitis, and cirrhosis. It helps your care team detect changes in your liver over time and guide treatment decisions — without the need for surgery or sedation.
-
Upper GI Endoscopy
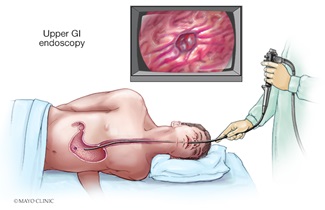
Overview
Also known as esophagogastroduodenoscopy (EGD) or gastroscopy, this procedure uses a small, flexible instrument to examine the esophagus, stomach and upper small intestine.
Why it's done
An EGD is done to look for causes of abdominal pain, difficult or painful swallowing, gastrointestinal bleeding, nausea and vomiting, heartburn and weight loss. During an EGD, your physician can dilate or stretch narrowed areas of the esophagus and stomach; take tissue samples (biopsies) to check for inflammation, infection and cancer; remove growths; remove foreign bodies or food that are stuck in the GI tract; find and treat actively bleeding lesions using medications, cautery or clipping devices.