without back pain
Spine Care
Spine Treatments in Menomonie
When you're experiencing back or neck pain, we'll ensure you see the right spine specialists at the right time. Together, we create an individualized plan so you can take control of your pain and start enjoying life again.
Spine treatments offered include:
Manual therapy
Treatments such as osteopathic manual medicine, chiropractic manipulation or soft tissue mobilization techniques commonly offered in physical therapy settings can be effective in acute and subacute episodes of back and neck pain to reduce pain and improve overall function.
Medications
Recommended medications depend on your type of back pain and can include:
- Pain relievers
Nonsteroidal anti-inflammatory drugs, or NSAIDs, such as ibuprofen (Advil, Motrin, others) or naproxen sodium (Aleve), and acetaminophen (Tylenol) might provide relief for episodic pain. Take these medications only as directed. Overuse can cause serious side effects. If over-the-counter pain relievers don't help, your healthcare provider might suggest prescription medications. - Muscle relaxants
If mild-to-moderate back pain doesn't improve with pain relievers, a muscle relaxant might help. These medications can cause dizziness and sleepiness. - Topical pain relievers
These products, including creams, salves, ointments and patches, deliver pain-relieving substances through the skin. Examples include mentholated or anti-inflammatory creams.
Physical therapy
A physical therapist teaches you exercises to increase flexibility, strengthen back and abdominal muscles, and improve posture. Regular use of these techniques can help keep pain from returning. They also provide education on how to modify movements when experiencing back pain to avoid making it worse during physical activity.
Nonsurgical procedures
When medication and therapy aren't enough, one of these nonsurgical procedures may be recommended:
- Basivertebral nerve ablation
This minimally invasive treatment can help relieve lower back pain caused by a specific type of pain coming from the vertebral bones and is an option after trying medications, physical therapy, weight control and other noninvasive therapies. The physician uses radiofrequency energy to destroy the nerve causing the pain, which stops pain signals from reaching your brain. - Epidural injection
During epidural injections, medication is injected directly into the epidural space surrounding your spinal cord. The epidural space is the sleeve that projects your spinal cord and is made up of fat, spinal nerves, blood vessels, and connective tissue. The injection acts on the nerves that is causing pain and reduces the surrounding swelling and pressure. Similar to fluoroscopic guided joint injections, the procedure is usually done using contrast dye to ensure the injection is given in the exact placement needed. - Interspinous distraction device implantation
This minimally invasive outpatient procedure can treat pain in your lower back, buttocks or legs caused by lumbar spinal stenosis. The physician implants a small metallic spacer between the bones in the spine to keep those bones spread apart, known as distraction. Distraction can relieve compression in various parts of the spinal canal. This procedure does not require general anesthesia. - Joint injection
These injections are given directly into the joint to help relieve pain. The procedure uses ultrasound-guided or fluoroscopic imaging using live X-ray with contrast dye to help your provider administer the medication in the exact placement needed. - Medial branch nerve block injection
These injections are used to help diagnose pain caused by the facet joints of the spine, which are the small joints in the spine that provide flexibility and stability. Medial branch nerves are responsible for carrying pain signals from the facet joints to the brain. Medial branch injections utilize X-ray or ultrasound technology and contrast dye to inject medication directly onto the medial branch nerves, temporarily blocking the nerves' ability to send pain signals to the brain. - Minimally invasive lumbar decompression
This outpatient procedure can treat pain in your lower back, buttocks or legs caused by lumbar spinal stenosis. During the procedure, the physician removes pieces of bone and ligament through a tiny incision in your back to restore the space in the spinal canal and relieve the compression on the nerves. This procedure doesn't require general anesthesia or stitches. - Peripheral nerve stimulation
This nerve stimulation device can often help treat chronic pain involving a focused body area, which not always is associated with a nerve injury. The physician implants one or more small electrical wires next to peripheral nerves. These wires attach to an external stimulator. When pain relief is needed, patients use an external device to produce and send electrical pulses from the stimulator to the nerves. - Radiofrequency ablation
Pain caused by the facet joints can be treated with radiofrequency ablation of the small nerves that supply the facet joints. To determine if this treatment is appropriate, a series of test blocks, referred to as medial branch nerve blocks or MBB, are completed. During a radiofrequency ablation procedure, a special needle and probe are placed next to medial branch nerves of interest. After application of a numbing medication, heat is applied through the needle, which damages the nerves, preventing them from sending pain signals to the brain. The procedure can provide durable relief lasting for many months and can be repeated if necessary. - Restorative neuromodulation
This minimally invasive procedure can help correct muscle deterioration and movement challenges related to lower back pain. The physician implants a device that will stimulate nerves, causing muscle contractions in the lower back. This restores strength to the muscles that stabilize the lower back and helps reduce pain. Patients use an external device to control daily therapy sessions. - Spinal cord stimulation
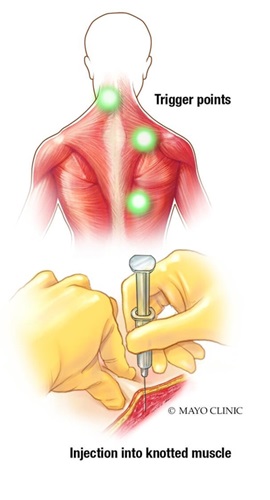
This nerve stimulation device can help reduce chronic pain and reliance on medications. The physician implants stimulation wires and a small generator (battery) under the skin, similar to a pacemaker. The generator delivers mild electrical pulses to the spinal cord to reduce the pain signals that travel through the spinal cord to the brain. - Trigger point injection
A trigger point injection may be an option if your back or neck pain is attributed to a small bump, nodule, or knot in your muscle, otherwise known as a trigger point. A trigger point is a band of tight muscle that can form after injury or overuse. During the procedure, a thin needle is injected directly into the trigger point. The injection aims to break up the knot in the muscle and provide relief from the pain and tension.
Surgical procedures
As a final resort, one of these surgical procedures may be recommended:
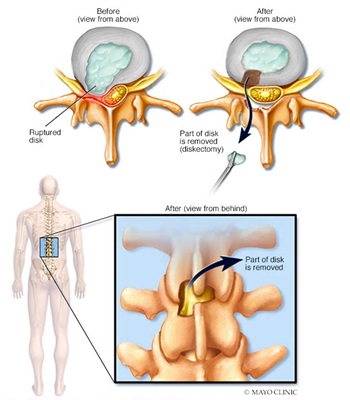
- Diskectomy
This surgical procedure removes the damaged portion of a herniated disk in your spine, which can irritate or compress nearby nerves. Diskectomy is most effective for treating pain that radiates down your arms or legs. It's performed to relieve the pressure a herniated disk — also called a slipped, ruptured or bulging disk, or disk prolapse — places on a spinal nerve.
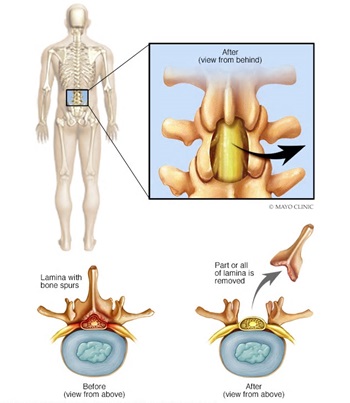
- Laminectomy
This surgery creates space by removing the lamina, which is the back part of a vertebra that covers your spinal canal. Also known as decompression surgery, laminectomy enlarges your spinal canal to relieve pressure on the spinal cord or nerves. This pressure most commonly is caused by bony overgrowths within the spinal canal, which can occur if you have arthritis in your spine. These overgrowths sometimes are referred to as bone spurs, but they're a normal side effect of the aging process in some people. Some patients are able to have a same-day laminectomy, which means they do not need to stay in the hospital following surgery and are able to go home to recover. The procedure is performed using minimally invasive techniques resulting in smaller incisions, lower risk of infection and, for many people, a quicker recovery.
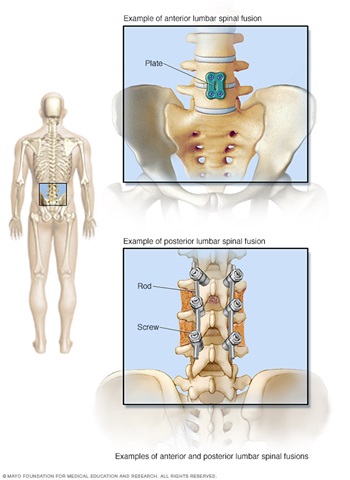
- Spinal fusion
This surgery permanently connects two or more vertebrae in your spine, eliminating abnormal or excessive motion between them. Spinal fusion involves techniques designed to mimic the normal healing process of broken bones. During spinal fusion, your surgeon places bone or a bone-like material within the space between two spinal vertebrae. Metal plates, screws and rods may be used to hold the vertebrae together so they can heal into one solid unit. Because spinal fusion surgery immobilizes parts of your spine, it changes the way your spine can move. This places additional stress and strain on the vertebrae above and below the fused portion, and may increase the rate at which those areas of your spine degenerate.